- Patient Care & Health Information
- Tests & Procedures
- Feminizing surgery
Feminizing surgery, also called gender-affirming surgery, involves procedures that help better align the body with a person's gender identity. Research has found that gender-affirming surgery can have a positive impact on well-being and sexual function.
Feminizing surgery includes several options, such as top surgery to increase the size of the breasts. That procedure also is called breast augmentation. Bottom surgery can involve removal of the testicles, or removal of the testicles and penis and the creation of a vagina, labia and clitoris. Facial procedures or body-contouring procedures can be used as well.
Not everybody chooses to have feminizing surgery. These surgeries can be expensive, carry risks and complications, and involve follow-up medical care and procedures. Certain surgeries change fertility and sexual sensations.
Your healthcare team can talk with you about your options and help you weigh the risks and benefits.

Products & Services
- A Book: Mayo Clinic Family Health Book
- Available Sexual Health Solutions at Mayo Clinic Store
- Newsletter: Mayo Clinic Health Letter — Digital Edition
Why it's done
Many people seek feminizing surgery as a step in the process of treating discomfort or distress because their gender identity differs from their sex assigned at birth. This is called gender dysphoria.
For some people, having feminizing surgery feels like a natural step. It's important to their sense of self. Others choose not to have surgery. All people relate to their bodies differently and should make individual choices that best suit their needs.
Feminizing surgery may include:
- Removal of the testicles alone. This is called orchiectomy.
- Removal of the penis, called penectomy.
- Removal of the testicles.
- Creation of a vagina, called vaginoplasty.
- Creation of a clitoris, called clitoroplasty.
- Creation of labia, called labioplasty.
- Breast surgery. Surgery to increase breast size is called top surgery or breast augmentation. It can be done through implants, the placement of tissue expanders under breast tissue, or the transplantation of fat from other parts of the body into the breast.
- Plastic surgery on the face. This is called facial feminization surgery. It involves plastic surgery techniques in which the jaw, chin, cheeks, forehead, nose, and areas surrounding the eyes, ears or lips are changed to create a more feminine appearance.
- Tummy tuck, called abdominoplasty.
- Buttock lift, called gluteal augmentation.
- Liposuction, a surgical procedure that uses a suction technique to remove fat from specific areas of the body.
- Voice feminizing therapy and surgery. These are techniques used to raise voice pitch.
- Tracheal shave. This surgery reduces the thyroid cartilage, also called the Adam's apple.
- Scalp hair transplant. This procedure removes hair follicles from the back and side of the head and transplants them to balding areas.
- Hair removal. A laser can be used to remove unwanted hair. Another option is electrolysis. It involves inserting a tiny needle into each hair follicle. The needle emits a pulse of electric current that damages and eventually destroys the follicle.
Like any other type of major surgery, many types of feminizing surgery pose a risk of bleeding, infection and a reaction to anesthetic. Depending on the procedures, other health concerns that might happen due to feminizing surgery include:
- Delayed wound healing.
- Fluid buildup beneath the skin, called seroma.
- Bruising, also called hematoma.
- Changes in skin sensation such as pain that doesn't go away, tingling, reduced sensation or numbness.
- Damaged or dead body tissue — a condition known as tissue necrosis — such as in the surgically created vagina or labia.
- A blood clot in a deep vein, called deep vein thrombosis, or a blood clot in the lung, called pulmonary embolism.
- Development of an irregular connection between two body parts, called a fistula, such as between the bladder or bowel into the vagina.
- Urinary problems, such as incontinence.
- Pelvic floor problems.
- Permanent scarring.
- Loss of sexual pleasure or function.
- Worsening of a behavioral health problem.
Certain types of feminizing surgery may limit or end fertility. If you want to have biological children and you're having surgery that involves your reproductive organs, talk with your healthcare professional before surgery. You may be able to freeze sperm with a technique called sperm cryopreservation.
How you prepare
Before surgery, you meet with your surgeon. Work with a surgeon who is board certified and experienced in the procedures you want. Your surgeon talks with you about your options and the potential results. The surgeon also may provide information on details such as the type of anesthesia that will be used during surgery and the kind of follow-up care that you may need.
Follow your healthcare team's directions on preparing for your procedures. This may include guidelines on eating and drinking. You may need to make changes in the medicine you take. Before surgery, you also may need to stop using nicotine, including vaping, smoking and chewing tobacco.
Because feminizing surgery might cause physical changes that cannot be reversed, you must give informed consent after thoroughly discussing:
- Risks and benefits.
- Alternatives to surgery, if applicable.
- Expectations and goals.
- Potential complications.
- Impact on sexual function and fertility.
Evaluation for surgery
Before surgery, a healthcare professional evaluates your health to address any medical conditions that might prevent you from having surgery or that could affect the procedure. This evaluation may be done by a health professional with expertise in transgender medicine. The evaluation might include:
- A review of your personal and family medical history.
- A physical exam.
- A review of any hormone therapy you've had.
- A review of your vaccinations.
- Screening tests for some conditions and diseases.
- Identification and management, if needed, of tobacco use, drug use, alcohol use disorder, and HIV or other sexually transmitted infections.
- Discussion about birth control, fertility and sexual function.
You also may have a behavioral health evaluation by a healthcare professional with expertise in transgender health. That evaluation might assess:
- Gender dysphoria.
- Mental health concerns.
- Sexual health concerns.
- The impact of gender dysphoria at work, at school, at home and in social settings.
- Substance use or use of hormone therapy or supplements not recommended by a health professional.
- Support from family, friends and caregivers.
- Your goals and expectations of treatment.
- Care planning and follow-up after surgery.
Other considerations
Health insurance coverage for feminizing surgery varies widely. Before you have surgery, check with your insurance provider to see what will be covered.
Before surgery, you might consider talking with others who have had feminizing surgery. If you don't know someone, ask your healthcare professional about support groups in your area or online resources you can trust. People who have gone through the process may be able to help you set your expectations and offer a point of comparison for your own goals of the surgery.
What you can expect
Facial feminization surgery.
Facial feminization surgery may involve a range of procedures to change facial features, including:
- Moving the hairline to create a smaller forehead.
- Enlarging the lips and cheekbones with implants.
- Reshaping the jaw and chin.
- Undergoing skin-tightening surgery after bone reduction.
These surgeries are typically done on an outpatient basis, so you don't have to stay in a hospital overnight. Recovery time for most of them is several weeks. Recovering from jaw procedures takes longer.
Tracheal shave
A tracheal shave minimizes the thyroid cartilage, also called the Adam's apple. During this procedure, a small cut is made under the chin, in the shadow of the neck or in a skin fold to conceal the scar. The surgeon then reduces and reshapes the cartilage. This is typically an outpatient procedure, requiring no hospital stay.
Top surgery
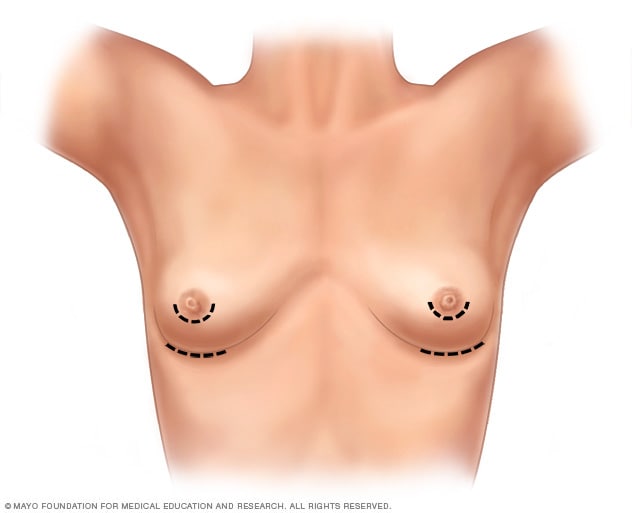
- Breast augmentation incisions
As part of top surgery, the surgeon makes cuts around the areola, near the armpit or in the crease under the breast.
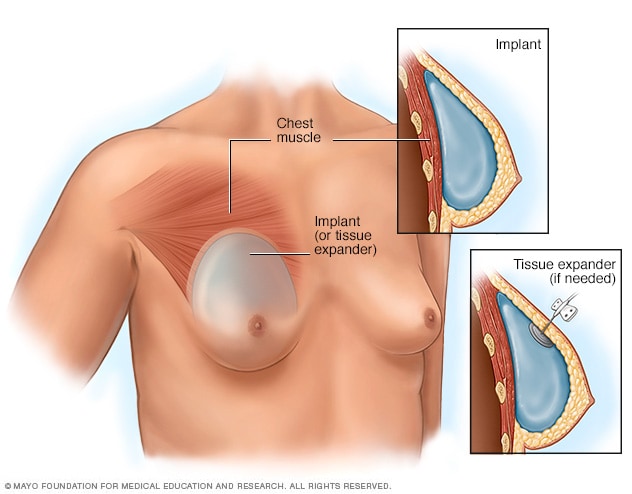
- Placement of breast implants or tissue expanders
During top surgery, the surgeon places the implants under the breast tissue. If feminizing hormones haven't made the breasts large enough, an initial surgery might be needed to have devices called tissue expanders placed in front of the chest muscles.
Hormone therapy with estrogen stimulates breast growth, but many people aren't satisfied with that growth alone. Top surgery is a surgical procedure to increase breast size that may involve implants, fat grafting or both.
During this surgery, a surgeon makes cuts around the areola, near the armpit or in the crease under the breast. Next, silicone or saline implants are placed under the breast tissue. Another option is to transplant fat, muscles or tissue from other parts of the body into the breasts.
If feminizing hormones haven't made the breasts large enough for top surgery, a surgery may be needed first to place devices called tissue expanders in front of the chest muscles. After that surgery, visits to a healthcare professional are needed every few weeks to have a small amount of saline injected into the tissue expanders. This slowly stretches the chest skin and other tissues to make room for the implants. When the skin has been stretched enough, another surgery is done to remove the expanders and place the implants.
Genital surgery
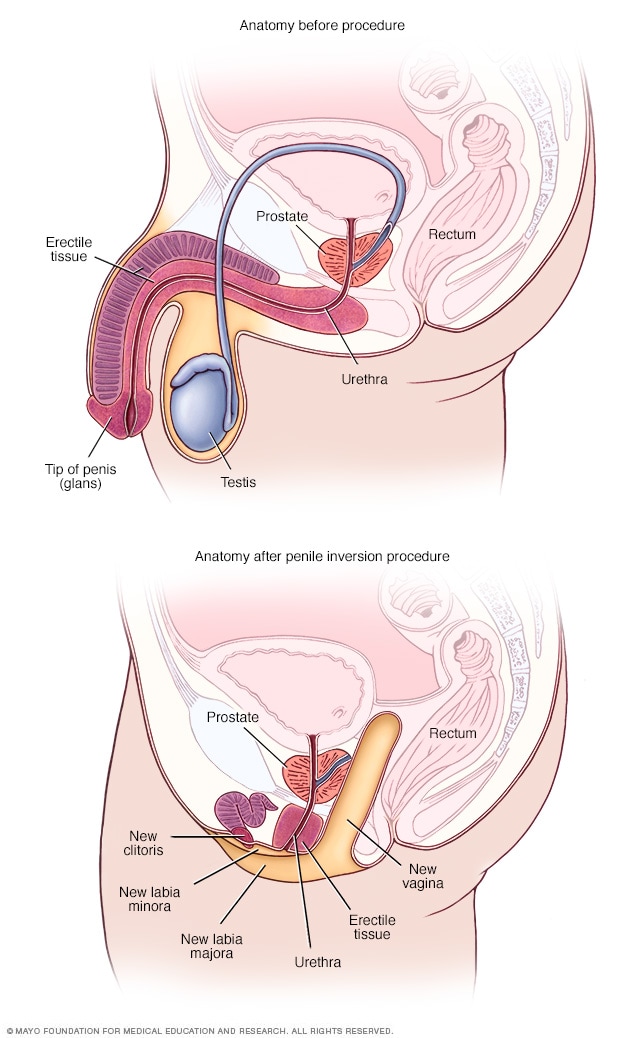
- Anatomy before and after penile inversion
During penile inversion, the surgeon makes a cut in the area between the rectum and the urethra and prostate. This forms a tunnel that becomes the new vagina. The surgeon lines the inside of the tunnel with skin from the scrotum, the penis or both. If there's not enough penile or scrotal skin, the surgeon might take skin from another area of the body and use it for the new vagina as well.
Orchiectomy
Orchiectomy is a surgery to remove the testicles. Because testicles make sperm and the hormone testosterone, an orchiectomy might eliminate the need to use testosterone blockers. It also may lower the amount of estrogen needed to achieve and maintain the appearance you want.
This type of surgery typically does not require a hospital stay. A local anesthetic may be used, so only the testicular area is numbed. Or the surgery may be done using general anesthesia. This means you are in a sleep-like state during the procedure.
To remove the testicles, a surgeon makes a cut in the scrotum and removes the testicles through the opening. Orchiectomy is done as part of the surgery for vaginoplasty. But some people prefer to have it done alone without other genital surgery.
Vaginoplasty
Vaginoplasty is the surgical creation of a vagina. During vaginoplasty, skin from the shaft of the penis and the scrotum is used to create a vaginal canal. This surgical approach is called penile inversion. In some techniques, the skin also is used to create the labia. That procedure is called labiaplasty. Labiaplasty is sometimes done without creation of a vaginal canal. This is called zero-depth vaginoplasty.
To surgically create a clitoris, a surgeon uses the tip of the penis and the nerves that supply it. This procedure is called a clitoroplasty. In some people, skin can be taken from another area of the body or tissue from the colon may be used to create the vagina. During vaginoplasty, the testicles are removed if that hasn't been done before.
Most surgeons require laser hair removal in the area of the penis and scrotum to provide hair-free tissue for the procedure. That process can take several months.
After vaginoplasty, a tube called a catheter is placed in the urethra to collect urine for several days. You need to be closely watched for about a week after surgery. Recovery can take up to two months. Your healthcare professional gives you instructions about when you may begin sexual activity with your new vagina.
After surgery, you're given a set of vaginal dilators of increasing sizes. You insert the dilators in your vagina to maintain, lengthen and stretch it. Follow your healthcare professional's directions on how often to use the dilators. To keep the vagina open, dilation needs to continue long term.
Because the prostate gland isn't removed during surgery, you need to follow age-appropriate recommendations for prostate cancer screening. Following surgery, it is possible to develop urinary symptoms from enlargement of the prostate.
Dilation after gender-affirming surgery
This material is for your education and information only. This content does not replace medical advice, diagnosis and treatment. If you have questions about a medical condition, always talk with your health care provider.
Narrator: Vaginal dilation is important to your recovery and ongoing care. You have to dilate to maintain the size and shape of your vaginal canal and to keep it open.
Jessi: I think for many trans women, including myself, but especially myself, I looked forward to one day having surgery for a long time. So that meant looking up on the internet what the routines would be, what the surgery entailed. So I knew going into it that dilation was going to be a very big part of my routine post-op, but just going forward, permanently.
Narrator: Vaginal dilation is part of your self-care. You will need to do vaginal dilation for the rest of your life.
Alissa (nurse): If you do not do dilation, your vagina may shrink or close. If that happens, these changes might not be able to be reversed.
Narrator: For the first year after surgery, you will dilate many times a day. After the first year, you may only need to dilate once a week. Most people dilate for the rest of their life.
Jessi: The dilation became easier mostly because I healed the scars, the stitches held up a little bit better, and I knew how to do it better. Each transgender woman's vagina is going to be a little bit different based on anatomy, and I grew to learn mine. I understand, you know, what position I needed to put the dilator in, how much force I needed to use, and once I learned how far I needed to put it in and I didn't force it and I didn't worry so much on oh, did I put it in too far, am I not putting it in far enough, and I have all these worries and then I stress out and then my body tenses up. Once I stopped having those thoughts, I relaxed more and it was a lot easier.
Narrator: You will have dilators of different sizes. Your health care provider will determine which sizes are best for you. Dilation will most likely be painful at first. It's important to dilate even if you have pain.
Alissa (nurse): Learning how to relax the muscles and breathe as you dilate will help. If you wish, you can take the pain medication recommended by your health care team before you dilate.
Narrator: Dilation requires time and privacy. Plan ahead so you have a private area at home or at work. Be sure to have your dilators, a mirror, water-based lubricant and towels available. Wash your hands and the dilators with warm soapy water, rinse well and dry on a clean towel. Use a water-based lubricant to moisten the rounded end of the dilators. Water-based lubricants are available over-the-counter. Do not use oil-based lubricants, such as petroleum jelly or baby oil. These can irritate the vagina. Find a comfortable position in bed or elsewhere. Use pillows to support your back and thighs as you lean back to a 45-degree angle. Start your dilation session with the smallest dilator. Hold a mirror in one hand. Use the other hand to find the opening of your vagina. Separate the skin. Relax through your hips, abdomen and pelvic floor. Take slow, deep breaths. Position the rounded end of the dilator with the lubricant at the opening to your vaginal canal. The rounded end should point toward your back. Insert the dilator. Go slowly and gently. Think of its path as a gentle curving swoop. The dilator doesn't go straight in. It follows the natural curve of the vaginal canal. Keep gentle down and inward pressure on the dilator as you insert it. Stop when the dilator's rounded end reaches the end of your vaginal canal. The dilators have dots or markers that measure depth. Hold the dilator in place in your vaginal canal. Use gentle but constant inward pressure for the correct amount of time at the right depth for you. If you're feeling pain, breathe and relax the muscles. When time is up, slowly remove the dilator, then repeat with the other dilators you need to use. Wash the dilators and your hands. If you have increased discharge following dilation, you may want to wear a pad to protect your clothing.
Jessi: I mean, it's such a strange, unfamiliar feeling to dilate and to have a dilator, you know to insert a dilator into your own vagina. Because it's not a pleasurable experience, and it's quite painful at first when you start to dilate. It feels much like a foreign body entering and it doesn't feel familiar and your body kind of wants to get it out of there. It's really tough at the beginning, but if you can get through the first month, couple months, it's going to be a lot easier and it's not going to be so much of an emotional and uncomfortable experience.
Narrator: You need to stay on schedule even when traveling. Bring your dilators with you. If your schedule at work creates challenges, ask your health care team if some of your dilation sessions can be done overnight.
Alissa (nurse): You can't skip days now and do more dilation later. You must do dilation on schedule to keep vaginal depth and width. It is important to dilate even if you have pain. Dilation should cause less pain over time.
Jessi: I hear that from a lot of other women that it's an overwhelming experience. There's lots of emotions that are coming through all at once. But at the end of the day for me, it was a very happy experience. I was glad to have the opportunity because that meant that while I have a vagina now, at the end of the day I had a vagina. Yes, it hurts, and it's not pleasant to dilate, but I have the vagina and it's worth it. It's a long process and it's not going to be easy. But you can do it.
Narrator: If you feel dilation may not be working or you have any questions about dilation, please talk with a member of your health care team.
Gender-affirming surgery can have a positive impact on well-being and sexual function. It's important to follow your healthcare professional's advice for long-term care and follow-up after surgery. Continued care after surgery is associated with good outcomes for long-term health.
Before you have surgery, talk with members of your healthcare team about what to expect after surgery and the ongoing care you may need.
Clinical trials
Explore Mayo Clinic studies of tests and procedures to help prevent, detect, treat or manage conditions.
Feminizing surgery care at Mayo Clinic
- Tangpricha V, et al. Transgender women: Evaluation and management. https://www.uptodate.com/ contents/search. Accessed Aug. 16, 2022.
- Erickson-Schroth L, ed. Surgical transition. In: Trans Bodies, Trans Selves: A Resource by and for Transgender Communities. 2nd ed. Kindle edition. Oxford University Press; 2022. Accessed Aug. 17, 2022.
- Coleman E, et al. Standards of care for the health of transgender and gender diverse people, version 8. International Journal of Transgender Health. 2022; doi:10.1080/26895269.2022.2100644.
- AskMayoExpert. Gender-affirming procedures (adult). Mayo Clinic; 2022.
- Nahabedian, M. Implant-based breast reconstruction and augmentation. https://www.uptodate.com/contents/search. Accessed Aug. 17, 2022.
- Erickson-Schroth L, ed. Medical transition. In: Trans Bodies, Trans Selves: A Resource by and for Transgender Communities. 2nd ed. Kindle edition. Oxford University Press; 2022. Accessed Aug. 17, 2022.
- Ferrando C, et al. Gender-affirming surgery: Male to female. https://www.uptodate.com/contents/search. Accessed Aug. 17, 2022.
- Anatomy before and after bowel flap procedure
- Gender dysphoria
- Doctors & Departments
- Care at Mayo Clinic
Mayo Clinic does not endorse companies or products. Advertising revenue supports our not-for-profit mission.
- Opportunities
Mayo Clinic Press
Check out these best-sellers and special offers on books and newsletters from Mayo Clinic Press .
- NEW: Listen to Health Matters Podcast - Mayo Clinic Press NEW: Listen to Health Matters Podcast
- Mayo Clinic on Incontinence - Mayo Clinic Press Mayo Clinic on Incontinence
- The Essential Diabetes Book - Mayo Clinic Press The Essential Diabetes Book
- Mayo Clinic on Hearing and Balance - Mayo Clinic Press Mayo Clinic on Hearing and Balance
- FREE Mayo Clinic Diet Assessment - Mayo Clinic Press FREE Mayo Clinic Diet Assessment
- Mayo Clinic Health Letter - FREE book - Mayo Clinic Press Mayo Clinic Health Letter - FREE book
Fund research. Save lives.
Benefactor support fuels Mayo Clinic’s groundbreaking research. Make a gift today to help us save lives.
Health Conditions
- Alzheimer's & Dementia
- Asthma & Allergies
- Atopic Dermatitis
- Breast Cancer
- Cardiovascular Health
- Environment & Sustainability
- Exercise & Fitness
- Headache & Migraine
- Health Equity
- HIV & AIDS
- Human Biology
- Men's Health
- Mental Health
- Multiple Sclerosis (MS)
- Parkinson's Disease
- Psoriatic Arthritis
- Sexual Health
- Ulcerative Colitis
- Women's Health
Health Products
- Nutrition & Fitness
- Vitamins & Supplements
- At-Home Testing
- Men’s Health
- Women’s Health
- Latest News
Original Series
- Medical Myths
- Honest Nutrition
- Through My Eyes
- New Normal Health
- Brain health, sleep, diet: 3 health resolutions for 2025
- 5 things everyone should know about menopause
- 3 ways to slow down type 2 diabetes-related brain aging
- Toxic metals in tampons: Should you be worried?
- Can tattoos cause blood or skin cancer?
- Can we really ‘outrun the Grim Reaper’?
General Health
- Health Hubs
Health Tools
- Find a Doctor
- BMI Calculators and Charts
- Blood Pressure Chart: Ranges and Guide
- Breast Cancer: Self-Examination Guide
- Sleep Calculator
- RA Myths vs Facts
- Type 2 Diabetes: Managing Blood Sugar
- Ankylosing Spondylitis Pain: Fact or Fiction
About Medical News Today
- Our Editorial Process
- Content Integrity
- Conscious Language
Find Community
- Bezzy Breast Cancer
- Bezzy Psoriasis
What to know about gender affirmation surgeries

Gender affirming surgeries (GAS) can help a person feel more comfortable and live as their most authentic self. They involve using surgical procedures to change a person’s appearance.
Everyone has a sense of their own gender identity, which may lie anywhere along a broad spectrum, and each person may choose to express their identity in different ways.
For people whose gender identity does not align with their sex assigned at birth, such as people within the transgender or gender-diverse community, being able to express their gender is important for their ability to feel safe, valid, and comfortable.
This article looks at different types of GAS, the preparation and recovery times for these procedures, and questions to ask a doctor.
Types of GAS

Some people may feel that surgery would not help them in expressing their gender identity , while others may choose to undergo a combination of procedures.
GAS can focus on many different areas of the body, including the:
- face and hair
Healthcare professionals may talk about these surgeries in terms of masculinizing and feminizing. While some people may identify with these terms, a person can have any mix of procedures regardless of their gender.
People may refer to GAS that focuses on the chest area as “top surgery,” and surgeries that focus on the genitals as “bottom surgery.”
Top surgeries
Top surgeries aim to reshape the chest in a way that affirms a person’s gender.
Top surgery procedures that aim to remove tissue and flatten the chest, sometimes known as masculinizing top surgeries, include :
- Double incision: This involves removing tissue from two incisions under the chest area.
- Periareolar: This involves making a circular incision around the areola, the skin circling the nipple, and working under the skin to remove tissue. Surgeons also make another incision to remove excess skin and reshape the areola. This procedure is best suited for smaller chests.
- Keyhole: To perform this procedure, surgeons use one small half-moon incision around the areola to remove tissue. Keyhole surgery does not include removing excess tissue or reshaping the areola. The procedure is best for small chests.
- Inverted-T: This procedure is similar to a double incision but keeps the nipple and areola attached to the nerves. This involves creating an extra incision from the nipples down to the horizontal double incisions, creating an upside-down “T” shape.
Top surgeries that aim to give the chest a fuller, rounder appearance typically involve breast augmentation using either saline or silicone implants.
Bottom surgeries
Bottom surgeries aim to make changes to the genitals to affirm a person’s gender.
Transfeminine bottom surgery
Transfeminine bottom surgery, also known as vaginal construction or vaginoplasty, refers to a procedure that reconstructs tissue from the penis and scrotum into a vaginal canal, clitoris, and labia.
A 2021 paper found transfeminine bottom surgeries have:
- a low rate of serious complications
- a high level of functionality
- high levels of satisfaction with the results
Transmasculine bottom surgeries
Transmasculine bottom surgeries, or penile construction surgeries, involve removal of the vagina and reconstruction of a penis and urethra.
The surgeon does this either using vaginal tissue and creating the penis around the clitoris ( metoidioplasty ) or using tissue from other parts of the body, such as the thigh or forearm (phalloplasty).
Some people may also have surgeries to remove the following:
- fallopian tubes
Other gender affirming procedures
Other GAS procedures include :
- Facial feminizing surgeries: Facial feminizing surgeries aim to create feminine facial features and can involve surgery on the nose, brow, chin, and jaw. Some people may also undergo hairline restoration and Adam’s apple reduction surgery.
- Facial masculinizing surgery: Facial masculinizing surgeries aim to create masculine facial features involving changes to the nose, forehead, chin, and jawline.
- Body contouring: Body contouring procedures aim to create a body shape that more closely aligns with a person’s gender. Procedures may involve either liposuction or fat crafting around the hips, abdomen, and buttocks to minimize or accentuate body curves.
What to expect from GAS procedures
GAS can be an emotionally charged experience.
A person may feel excited but overwhelmed by the thought of undergoing such procedures. People may benefit from having an understanding support system around them to help them through this process and their recovery.
Although everyone’s journey is different, a person may find talking with others who have undergone similar surgeries helpful. They can also speak with a doctor about what to expect and any concerns they may have.
The National Center for Trans Equality offers a list of healthcare and mental health resources that can provide individuals with extra support during their gender affirming process.
As for physical preparation, some specialists may recommend that a person be on hormone therapy for a certain period before surgery.
Candidates for GAS
When working with a person to see if they would be a good candidate for GAS, many specialists follow the World Professional Association for Transgender Health (WPATH) guidelines.
WPATH suggests that it is best for a person undergoing GAS to meet the following criteria:
- They experience ongoing gender dysphoria .
- They have the ability to give informed consent for their treatment.
- They are considered an adult according to the laws in their country.
- Any existing mental health or medical problems they experience are well-managed.
Recovery from GAS
Recovery from GAS can vary depending on which procedures are involved. For example, healing from a vaginoplasty can take several weeks. A person will need to wait around 4 weeks before having penetrative sex.
The recovery period after facial feminizing surgery can also last several weeks . Individuals will need to follow all postoperative instructions from their surgeon.
It is best for people to speak with their surgeon about their recovery plan for the specific procedures they are having. Where possible, a person may wish to make arrangements for a friend or loved one to provide them with support and care at home for the first few days after surgery.
Questions to ask a doctor
During a consultation about GAS, a person may wish to ask their surgeon the following questions:
- Is the surgeon a member of WPATH?
- Can they show before and after pictures that give a reasonable expectation of results?
- How long is the recovery process, and what support is available?
- What are the risks and complications of the procedure?
- What are the steps for managing complications?
- What are the options if a person is dissatisfied with their results?
A person can find surgeons who are members of WPATH and trained in transgender medical care on the WPATH website .
Gender affirming surgery describes a range of procedures that aim to match a person’s outward appearance more closely with their gender identity.
GAS is an important part of healthcare for transgender and gender-diverse individuals. These life changing procedures can help a person feel physically aligned with their identity and allow them to live comfortably and happily as themselves.
There is no one right way to present gender. People may undergo different combinations of procedures, or they may not wish to have any surgeries.
How we reviewed this article:
- Additional help. (n.d.). https://transequality.org/additional-help
- Asokan A, et al. (2022). Gender affirming body contouring and physical transformation in transgender individuals. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9398519/
- Coleman E, et al. (2022). Standards of care for the health of transgender and gender diverse people, version 8. https://www.tandfonline.com/doi/pdf/10.1080/26895269.2022.2100644
- Feminizing chest surgery. (2019). https://actt.albertadoctors.org/media/domebfqf/feminizing-chest-surgery.pd
- Gender affirmation surgeries. (n.d.). https://www.plasticsurgery.org/reconstructive-procedures/gender-affirmation-surgeries
- Member search. (n.d.). https://www.wpath.org/member/search
- Moisés da Silva G V, et al. (2021). Male-to-female gender-affirming surgery: 20-year review of technique and surgical results. https://www.frontiersin.org/articles/10.3389/fsurg.2021.639430/full
- Selvaggi G, et al. (2018). Gender affirmation surgery. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6057344/
- Top surgery. (n.d.). https://www.transhub.org.au/top-surgery
- Vaginoplasty - feminising surgery. (2021). https://www.leedsandyorkpft.nhs.uk/our-services/wp-content/uploads/sites/2/2021/10/v3_vaginoplasty-leaflet_gender_dysphoria.pdf
Share this article
Latest news
- Intermittent fasting paired with exercise may be best for weight loss
- Why BMI is not the obesity measurement we need
- Mountain climbing and treating Alzheimer's: Could xenon gas have potential?
- How doctors may be able to predict your stroke risk through your eye
- Green tea drinkers have fewer brain lesions linked to dementia
Related Coverage
Transgender is a term to refer to those who have a different gender identity than the one assigned to them at birth. Learn more here.
There are different types of surgery for transgender men. Learn more about how long to wait until it is safe to have sex and other sexual health tips…
Transgender and transsexual have different definitions. Learn more about what they mean and the terminology to avoid here.
Coming out is an unique experience. Some people may find it easy to talk with those close to them, while others may find it challenging. Read more…
Gender stereotypes are generalised views about how people should behave or which characteristics they should have based on their gender. Read more…
- Type 2 Diabetes
- Heart Disease
- Digestive Health
- Multiple Sclerosis
- Diet & Nutrition
- Health Insurance
- Public Health
- Patient Rights
- Caregivers & Loved Ones
- End of Life Concerns
- Health News
- Thyroid Test Analyzer
- Doctor Discussion Guides
- Hemoglobin A1c Test Analyzer
- Lipid Test Analyzer
- Complete Blood Count (CBC) Analyzer
- What to Buy
- Editorial Process
- Meet Our Medical Expert Board
Preparation and Procedures Involved in Gender Affirmation Surgeries
If you or a loved one are considering gender affirmation surgery , you are probably wondering what steps you must go through before the surgery can be done. Let's look at what is required to be a candidate for these surgeries, the potential positive effects and side effects of hormonal therapy, and the types of surgeries that are available.
Gender affirmation surgery, also known as gender confirmation surgery, is performed to align or transition individuals with gender dysphoria to their true gender.
A transgender woman, man, or non-binary person may choose to undergo gender affirmation surgery.
The term "transexual" was previously used by the medical community to describe people who undergo gender affirmation surgery. The term is no longer accepted by many members of the trans community as it is often weaponized as a slur. While some trans people do identify as "transexual", it is best to use the term "transgender" to describe members of this community.
Transitioning
Transitioning may involve:
- Social transitioning : going by different pronouns, changing one’s style, adopting a new name, etc., to affirm one’s gender
- Medical transitioning : taking hormones and/or surgically removing or modifying genitals and reproductive organs
Transgender individuals do not need to undergo medical intervention to have valid identities.
Reasons for Undergoing Surgery
Many transgender people experience a marked incongruence between their gender and their assigned sex at birth. The American Psychiatric Association (APA) has identified this as gender dysphoria.
Gender dysphoria is the distress some trans people feel when their appearance does not reflect their gender. Dysphoria can be the cause of poor mental health or trigger mental illness in transgender people.
For these individuals, social transitioning, hormone therapy, and gender confirmation surgery permit their outside appearance to match their true gender.
Steps Required Before Surgery
In addition to a comprehensive understanding of the procedures, hormones, and other risks involved in gender-affirming surgery, there are other steps that must be accomplished before surgery is performed. These steps are one way the medical community and insurance companies limit access to gender affirmative procedures.
Steps may include:
- Mental health evaluation : A mental health evaluation is required to look for any mental health concerns that could influence an individual’s mental state, and to assess a person’s readiness to undergo the physical and emotional stresses of the transition.
- Clear and consistent documentation of gender dysphoria
- A "real life" test : The individual must take on the role of their gender in everyday activities, both socially and professionally (known as “real-life experience” or “real-life test”).
Firstly, not all transgender experience physical body dysphoria. The “real life” test is also very dangerous to execute, as trans people have to make themselves vulnerable in public to be considered for affirmative procedures. When a trans person does not pass (easily identified as their gender), they can be clocked (found out to be transgender), putting them at risk for violence and discrimination.
Requiring trans people to conduct a “real-life” test despite the ongoing violence out transgender people face is extremely dangerous, especially because some transgender people only want surgery to lower their risk of experiencing transphobic violence.
Hormone Therapy & Transitioning
Hormone therapy involves taking progesterone, estrogen, or testosterone. An individual has to have undergone hormone therapy for a year before having gender affirmation surgery.
The purpose of hormone therapy is to change the physical appearance to reflect gender identity.
Effects of Testosterone
When a trans person begins taking testosterone , changes include both a reduction in assigned female sexual characteristics and an increase in assigned male sexual characteristics.
Bodily changes can include:
- Beard and mustache growth
- Deepening of the voice
- Enlargement of the clitoris
- Increased growth of body hair
- Increased muscle mass and strength
- Increase in the number of red blood cells
- Redistribution of fat from the breasts, hips, and thighs to the abdominal area
- Development of acne, similar to male puberty
- Baldness or localized hair loss, especially at the temples and crown of the head
- Atrophy of the uterus and ovaries, resulting in an inability to have children
Behavioral changes include:
- Aggression
- Increased sex drive
Effects of Estrogen
When a trans person begins taking estrogen , changes include both a reduction in assigned male sexual characteristics and an increase in assigned female characteristics.
Changes to the body can include:
- Breast development
- Loss of erection
- Shrinkage of testicles
- Decreased acne
- Decreased facial and body hair
- Decreased muscle mass and strength
- Softer and smoother skin
- Slowing of balding
- Redistribution of fat from abdomen to the hips, thighs, and buttocks
- Decreased sex drive
- Mood swings
When Are the Hormonal Therapy Effects Noticed?
The feminizing effects of estrogen and the masculinizing effects of testosterone may appear after the first couple of doses, although it may be several years before a person is satisfied with their transition. This is especially true for breast development.
Timeline of Surgical Process
Surgery is delayed until at least one year after the start of hormone therapy and at least two years after a mental health evaluation. Once the surgical procedures begin, the amount of time until completion is variable depending on the number of procedures desired, recovery time, and more.
Transfeminine Surgeries
Transfeminine is an umbrella term inclusive of trans women and non-binary trans people who were assigned male at birth.
Most often, surgeries involved in gender affirmation surgery are broken down into those that occur above the belt (top surgery) and those below the belt (bottom surgery). Not everyone undergoes all of these surgeries, but procedures that may be considered for transfeminine individuals are listed below.
Top surgery includes:
- Breast augmentation
- Facial feminization
- Nose surgery: Rhinoplasty may be done to narrow the nose and refine the tip.
- Eyebrows: A brow lift may be done to feminize the curvature and position of the eyebrows.
- Jaw surgery: The jaw bone may be shaved down.
- Chin reduction: Chin reduction may be performed to soften the chin's angles.
- Cheekbones: Cheekbones may be enhanced, often via collagen injections as well as other plastic surgery techniques.
- Lips: A lip lift may be done.
- Alteration to hairline
- Male pattern hair removal
- Reduction of Adam’s apple
- Voice change surgery
Bottom surgery includes:
- Removal of the penis (penectomy) and scrotum (orchiectomy)
- Creation of a vagina and labia
Transmasculine Surgeries
Transmasculine is an umbrella term inclusive of trans men and non-binary trans people who were assigned female at birth.
Surgery for this group involves top surgery and bottom surgery as well.
Top surgery includes :
- Subcutaneous mastectomy/breast reduction surgery.
- Removal of the uterus and ovaries
- Creation of a penis and scrotum either through metoidioplasty and/or phalloplasty
Complications and Side Effects
Surgery is not without potential risks and complications. Estrogen therapy has been associated with an elevated risk of blood clots ( deep vein thrombosis and pulmonary emboli ) for transfeminine people. There is also the potential of increased risk of breast cancer (even without hormones, breast cancer may develop).
Testosterone use in transmasculine people has been associated with an increase in blood pressure, insulin resistance, and lipid abnormalities, though it's not certain exactly what role these changes play in the development of heart disease.
With surgery, there are surgical risks such as bleeding and infection, as well as side effects of anesthesia . Those who are considering these treatments should have a careful discussion with their doctor about potential risks related to hormone therapy as well as the surgeries.
Cost of Gender Confirmation Surgery
Surgery can be prohibitively expensive for many transgender individuals. Costs including counseling, hormones, electrolysis, and operations can amount to well over $100,000. Transfeminine procedures tend to be more expensive than transmasculine ones. Health insurance sometimes covers a portion of the expenses.
Quality of Life After Surgery
Quality of life appears to improve after gender-affirming surgery for all trans people who medically transition. One 2017 study found that surgical satisfaction ranged from 94% to 100%.
Since there are many steps and sometimes uncomfortable surgeries involved, this number supports the benefits of surgery for those who feel it is their best choice.
A Word From Verywell
Gender affirmation surgery is a lengthy process that begins with counseling and a mental health evaluation to determine if a person can be diagnosed with gender dysphoria.
After this is complete, hormonal treatment is begun with testosterone for transmasculine individuals and estrogen for transfeminine people. Some of the physical and behavioral changes associated with hormonal treatment are listed above.
After hormone therapy has been continued for at least one year, a number of surgical procedures may be considered. These are broken down into "top" procedures and "bottom" procedures.
Surgery is costly, but precise estimates are difficult due to many variables. Finding a surgeon who focuses solely on gender confirmation surgery and has performed many of these procedures is a plus. Speaking to a surgeon's past patients can be a helpful way to gain insight on the physician's practices as well.
For those who follow through with these preparation steps, hormone treatment, and surgeries, studies show quality of life appears to improve. Many people who undergo these procedures express satisfaction with their results.
Bizic MR, Jeftovic M, Pusica S, et al. Gender dysphoria: Bioethical aspects of medical treatment . Biomed Res Int . 2018;2018:9652305. doi:10.1155/2018/9652305
American Psychiatric Association. What is gender dysphoria? . 2016.
The World Professional Association for Transgender Health. Standards of care for the health of transsexual, transgender, and gender-nonconforming people . 2012.
Tomlins L. Prescribing for transgender patients . Aust Prescr . 2019;42(1): 10–13. doi:10.18773/austprescr.2019.003
T'sjoen G, Arcelus J, Gooren L, Klink DT, Tangpricha V. Endocrinology of transgender medicine . Endocr Rev . 2019;40(1):97-117. doi:10.1210/er.2018-00011
Unger CA. Hormone therapy for transgender patients . Transl Androl Urol . 2016;5(6):877-884. doi:10.21037/tau.2016.09.04
Seal LJ. A review of the physical and metabolic effects of cross-sex hormonal therapy in the treatment of gender dysphoria . Ann Clin Biochem . 2016;53(Pt 1):10-20. doi:10.1177/0004563215587763
Schechter LS. Gender confirmation surgery: An update for the primary care provider . Transgend Health . 2016;1(1):32-40. doi:10.1089/trgh.2015.0006
Altman K. Facial feminization surgery: current state of the art . Int J Oral Maxillofac Surg . 2012;41(8):885-94. doi:10.1016/j.ijom.2012.04.024
Therattil PJ, Hazim NY, Cohen WA, Keith JD. Esthetic reduction of the thyroid cartilage: A systematic review of chondrolaryngoplasty . JPRAS Open. 2019;22:27-32. doi:10.1016/j.jpra.2019.07.002
Top H, Balta S. Transsexual mastectomy: Selection of appropriate technique according to breast characteristics . Balkan Med J . 2017;34(2):147-155. doi:10.4274/balkanmedj.2016.0093
Chan W, Drummond A, Kelly M. Deep vein thrombosis in a transgender woman . CMAJ . 2017;189(13):E502-E504. doi:10.1503/cmaj.160408
Streed CG, Harfouch O, Marvel F, Blumenthal RS, Martin SS, Mukherjee M. Cardiovascular disease among transgender adults receiving hormone therapy: A narrative review . Ann Intern Med . 2017;167(4):256-267. doi:10.7326/M17-0577
Hashemi L, Weinreb J, Weimer AK, Weiss RL. Transgender care in the primary care setting: A review of guidelines and literature . Fed Pract . 2018;35(7):30-37.
Van de grift TC, Elaut E, Cerwenka SC, Cohen-kettenis PT, Kreukels BPC. Surgical satisfaction, quality of life, and their association after gender-affirming aurgery: A follow-up atudy . J Sex Marital Ther . 2018;44(2):138-148. doi:10.1080/0092623X.2017.1326190
American Society of Plastic Surgeons. Gender confirmation surgeries .
American Psychological Association. Transgender people, gender identity, and gender expression .
Colebunders B, Brondeel S, D'Arpa S, Hoebeke P, Monstrey S. An update on the surgical treatment for transgender patients . Sex Med Rev . 2017 Jan;5(1):103-109. doi:10.1016/j.sxmr.2016.08.001
Sexual Health
Weight Loss
Daily Health
Top Products
What We Treat
Gender reassignment surgery: what is it, how it works, recovery, cost
10 min read
Written by:
Nancy LaChance, BSN, RN
Reviewed by:
Steve Silvestro, MD, Ro
Updated: Feb 10, 2022
Here's what we'll cover
Many transgender individuals choose to align their bodies with their true gender identities through gender reassignment surgery. These surgeries can help relieve psychological distress and are often considered medically necessary. Many surgeries are available, and treatment is individualized depending on a person’s goals and needs.
How does gender reassignment surgery work, what are the side effects and complications, how much does it cost, and what recovery and results can you expect? Keep reading to find out.
Improve and support your health from the comfort of home
What is gender reassignment surgery?
Gender reassignment surgery—also called gender affirmation surgery, sex reassignment surgery, transgender surgery, and gender confirmation surgery—refers to several procedures that change the shape and function of a person’s genitalia (and potentially face and other features) to better align with their gender identity.
Many people choose to have these surgeries to relieve years of inner struggle with a body that does not match who they are inside. It’s estimated that there are around 1.5 million people who identify as transgender in the US (likely more), and thankfully, these surgeries are becoming increasingly common. Around 9,000 transgender surgical procedures (and counting) are performed every year ( Cohen, 2019 ; Mani, 2021 ).
Surgery is often part of a several-step process of gender affirmation. This process can include social changes (living in the desired gender role, coming out as transgender to family and friends, and changing pronoun use), legal name change, and physical changes (including changed clothing, hairstyles, and medical interventions like hormone therapy and surgery).
A transgender person can choose whichever combination of transition steps feels right for their goals and identity, including which (if any) surgical procedures are right for them. Not all transgender people need or want surgery, though many do.
Types of gender reassignment surgery
There are a few overlapping categories of gender reassignment surgery: surgery for male to female (MTF) transition and surgery for female to male (FTM) transition .
For FTM transitions, people may choose to have “top” surgery (chest surgery for breast removal and chest masculinization) and/or “bottom” surgery (female sex organ removal and penis creation surgery).
For MTF transitions, people may also choose to have “top” surgery (surgery to reshape the chest and place breast implants) and/or “bottom” surgery (male sex organ removal and vagina creation surgery) ( WPATH, 2012 ).
There are multiple surgical techniques possible for each type of surgery, and a person can develop a unique care plan with their doctor.

Vaginoplasty
Vaginoplasty is the surgical creation of a vagina for a transgender woman. It also generally includes removing the penis (penile dissection) and testicles (orchiectomy).
How it works
There are three main surgical methods of creating a vagina ( Chen, 2019 ):
Using genital skin
Using skin from an area of the body other than the genitals
Using a portion of the intestines
Using genital skin (the skin of the penis) is the most common method. It’s called the “penile inversion” method and is widely reported to have excellent results. It also allows a woman and her surgeon to decide what vaginal depth is right for her. Depending on what feels right for her, she can choose to have a full-depth vagina that allows for full sexual penetration or a partial- or zero-depth vagina (Chen, 2019).
Other surgeries, like a labiaplasty (creation of a labia), vulvoplasty (creation of a vulva), and clitoroplasty (creation of a clitoris) can be a part of a vaginoplasty procedure. The surgeon can use the head of the penis to create a clitoris and skin of the scrotum to create a labia and vulva, all of which can improve the sensation of the new vagina (Chen, 2019).
Before surgery, permanent hair removal from the penis and scrotum using laser hair removal or electrolysis is very important (if this tissue is going to be used to create the vagina). Hair removal helps prevent infection and issues with hair regrowth inside the new vagina. The surgery requires an inpatient hospital stay of roughly five days, allowing trained medical staff to keep a close eye on the early healing and wound draining ( Par iser, 2019 ).
Risks & recovery
Risks and complications with vaginoplasty using the penile inversion technique are relatively low. Most complications—problems with wound healing, rectal injury, damage to the urethra, and significant tissue death requiring follow-up surgery—occur in fewer than 5% of patients (Pariser, 2019).
After a vaginoplasty, the surgeon will prescribe therapy using vaginal dilators. Dilators promote stretching of the vaginal tissue, prevent the vagina from narrowing, and enable comfortable penetrative sex. This therapy, along with vaginal cleansing or douching, will have to be continued for the rest of the woman’s life. This may sound onerous, but it is pretty simple and important for ensuring the vagina stays healthy and functional (Pariser, 2019).
Vaginoplasty procedures tend to cost tens of thousands of dollars. However, more and more insurance companies are offering coverage for transgender health services; 97% of US insurance companies cover vaginoplasty, although only 21% cover vulvoplasty (Cohen, 2019). It’s best to speak with your insurance and the hospital or surgical practice you are considering to get a realistic sense of what the cost of surgery could be under your plan.
Breast augmentation
Breast augmentation is a surgery that many transgender women choose as part of the MTF transition. Thankfully, this procedure is more available in the US than genital reconfiguration surgery, as breast implant surgery has been widely practiced for many years in cis-gendered women (Chen, 2019). Many transwomen report that breast augmentation dramatically improves their self-image and quality of life. For many transwomen, it’s the only surgery they choose to undergo ( Bekeny, 2020 ).
Breast augmentation for gender reassignment surgery is very similar to breast augmentation or reconstruction in cisgendered individuals: implants filled with saline, silicone, or a person’s body fat are inserted either on top of or beneath the pectoral muscles of the chest ( Fardo, 2021 ). You can discuss with your doctor which method of breast augmentation they prefer and which is right for you.
The contours of the chest can also be reshaped to a more feminine form using fat grafting from the buttocks and hips. Surgeons also pay close attention to minimizing scarring and ensuring correct nipple position (Bekeny, 2020).
It’s recommended (but not required) for transgender women to undergo a year of hormone therapy before having breast augmentation surgery; this helps the chest produce as much soft tissue as possible and enhances the appearance of the augmented breasts after surgery (WPATH, 2012).
The risk of complications with breast augmentation is low, with only 1.8% of transgender patients experiencing bleeding, wound healing issues, infection, implant leakage, and reduced sensation in the breasts and nipples (Bekeny, 2020).
Breast augmentation costs around $6,000 out of pocket in the US ( Schmitt, 2016 ). Generally speaking, it’s still considered a cosmetic procedure, but as of 2019, nearly a third of US insurance companies covered “chest feminization” procedures for people with gender dysphoria (Cohen, 2019). If you’re considering breast augmentation for MTF transition, it’s a good idea to check with your insurance company and healthcare provider to see whether it could be covered under your plan.
Breast removal (mastectomy)
Breast reduction and removal (subcutaneous mastectomy), or FTM “top” surgery, is often chosen as the first surgical step by transgender men during their transition process. It’s shown to improve the quality of life for transgender men significantly, in aspects ranging from greater self-esteem and feelings of authenticity to better sexual enjoyment ( van de Grift, 2019 ; WPATH, 2012).
Subcutaneous mastectomy involves removing breast tissue and excess skin, flattening the shape of the chest, and repositioning the nipples on the chest to a typical and aesthetically appealing position. Surgeons strive to minimize scarring (although some scarring is inevitable), maintain nipple sensation, and reduce nipple size to a more typically masculine size. Surgeons use several different techniques, but patient satisfaction rates are high across the board ( Bustos, 2021 ).
Risks of the procedure are similar to other major surgeries, including bleeding and infection. However, a 2018 systematic review found that only 6% of patients had experienced problematic bleeding (a hematoma) requiring follow-up surgery ( Wilson, 2018 ). Top surgery is an outpatient procedure, and recovery typically takes 1–2 weeks.
Breast removal and chest masculinization surgery can be expensive out-of-pocket. Fortunately, nearly all (98%) of US health insurance companies cover it (although only 20% cover nipple-areolar complex reconstruction, which is a surgery to improve the cosmetics of the nipple size and position on the chest) (Cohen, 2019). It’s best to check with your insurance company and healthcare provider to see what your plan covers.
Phalloplasty
Phalloplasty is one method of surgically creating a penis, often part of FTM transition (it’s also done to reconstruct the penis after traumatic injury in cisgender men). There are several options and stages of this process, and your provider can tailor a care plan to your individual goals.
In phalloplasty , a new penis is created out of a person’s own skin and tissue. It’s surgically attached to the pelvis and can also be connected to the urethra so that the person can urinate standing up if they would like ( Heston, 2019 ).
There are two main phalloplasty techniques. The radial forearm free flap, or RFFF method, uses a flap of skin from the forearm to create the new penis. The anterolateral thigh, or ALT method, uses a flap of skin from the person’s thigh.
There are pros and cons to both of these methods. The RFFF method is usually preferred because the skin of the forearm is thin and sensitive—more similar to genital skin. This skin also has a good supply of nerves and blood vessels (so there is better blood flow and tactile sensation in the penis). The phalloplasty can usually be completed in only one or two surgeries with the RFFF method. However, it does leave a large and identifiable forearm scar, which some people don’t want ( Van Caenegem, 2013 ).
In this case, the ALT method may be an option. Since it uses skin from the thigh, the “donor site” scar is easier to conceal. It can also create a larger penis with slightly firmer tissue, which some people may prefer. However, the thigh's nerve and blood vessel supply are not as abundant as the forearm. There is often a lot of fatty tissue, so the penis can have less tactile sensitivity and usually requires follow-up surgery to decrease its size. More follow-up surgeries are necessary with the ALT method than the RFFF method (Chen, 2019).
Phalloplasty usually involves removal of some or all of the female sex organs, including the vagina (called a vaginectomy), uterus (a hysterectomy), and ovaries (an oophorectomy ). A patient may also have a phalloplasty without removing these organs. If you choose a hysterectomy or oophorectomy, it must usually be completed before the surgery to allow your body time to recover before the phalloplasty ( Carter, 2020 ).
Follow-up surgeries are often done to create a scrotum, correct issues with the urethra, improve penis aesthetics and create a glans (head of the penis), or place prosthetics that enable erections and sexual function (Chen, 2019).
Recovery from phalloplasty takes up to 12 weeks. There’s usually a five-day hospital stay, where your healthcare team will closely monitor you to watch for complications and to make sure the new penis has good blood flow.
Recovery at home takes 4–12 weeks, with weekly home visits from a healthcare provider for the first month or two. You’ll have a catheter in the urethra for the first week, then a catheter above the pubic bone for three weeks until you begin urinating normally. For at least the first month, you should limit big movements and all physical strain, even excessive walking and lifting. It’s also important to avoid bending deeply at the waist or putting pressure on the new penis (Carter, 2020).
Phalloplasty carries a significant risk of complications, although most patients are still pleased with the results of their surgery and would choose to do it again ( Papadopulos, 2021 ). Most patients have minor complications immediately following surgery (things like pain, bleeding, skin issues, and UTIs ), and about a third of patients experience a significant complication and need corrective surgery. These include strictures and fistulas (abnormal narrowing or holes) in the urethra, tissue death of the new penis, wound breakdown, and lack of sensation ( Ascha, 2018 ; Santucci, 2018 ).
Phalloplasties tend to cost several tens of thousands of dollars when paid for out of pocket. However, thanks to the Affordable Care Act and increasing awareness of transgender health needs, 95% of US insurance companies cover phalloplasty, and 60% cover penile prosthesis ( Baker, 2017 ; Cohen, 2019). It’s a good idea to speak with your insurance company and the hospital or surgical practice you are considering to get a realistic sense of what the cost could be.
Metoidioplasty
Metoidioplasty is another method of surgically creating a penis and is only done in a person with female anatomy (so, unlike phalloplasty, it isn’t a method of penis reconstruction used in cisgendered men).
In a metoidioplasty, a small penis is built using tissue from a person’s clitoris. During the surgery, the clitoris is “released” and extended outward. Other genital tissue from the person’s labia is used to build up a penis. Patients often opt for scrotoplasty as well, in which a small scrotal pouch is created from the labia. The procedure is completed in a single surgery unless the person has a complication or wants a later surgery for testicular implants (Chen, 2019).
As with a phalloplasty, a person can choose to reconstruct the urethra to try and enable urination while standing. However, the success of this can vary depending on how large the penis is; sometimes, they are too small to realistically enable urination while standing (Chen, 2019). Surgeons usually recommend that a person undergo masculinizing hormone therapy for at least a year before surgery, as this helps enlarge the clitoris as much as possible ( Jolly, 2021 ).
Because they use clitoral tissue (rather than tissue from a donor site elsewhere on the body), the ability to have spontaneous sexual blood flow usually enables the man to have erections. However, because the penis created in a metoidioplasty is small, it’s not a guarantee that he’ll be able to penetrate a partner during sex (though most people can) ( Jolly, 2021 ; van de Grift, 2019).
The risks of metoidioplasty are much lower than with a phalloplasty since it’s a less complex surgery. There are also no donor sites that need to heal, and reconstruction with the urethra tends to be less complicated because the penis shaft is shorter (Chen, 2019).
Metoidioplasty patients are usually discharged on the same day or watched overnight; the surgery rarely requires a long hospital stay. Recovery lasts for several weeks, and the patient is encouraged to walk gently but often. Some swelling of the penis and drainage is to be expected.
The main complications to watch out for are issues with urination. Fortunately, although about 25% of patients experience urethral complications, most of these resolve on their own and don’t require follow-up surgery (Chen, 2019).
Metoidioplasty procedures tend to cost ten thousand dollars or more out-of-pocket (though typically less than phalloplasty because the surgery is less complicated). Fortunately, 93% of US health insurance companies cover metoidioplasty. You can speak with your insurance company and the hospital or surgical practice you are considering to get a realistic sense of costs.
Key considerations
Before undergoing any surgery, it’s important to understand what to expect fully. With gender reassignment surgery, in particular, there are many considerations since it’s such a complex set of procedures with so many emotional, physical, and social implications. Here are some key things to be aware of as you embark on this journey:
Setting goals and expectations
Having a candid, honest talk with your healthcare provider about what you want from surgery and your risk tolerance can help increase the likelihood of having a satisfying and successful experience. Your provider can help make sure you have a good support system and realistic expectations about things like sensation, orgasm, and sexual pleasure . When these open discussions happen, rates of post-surgery disappointment are extremely low—a 2021 systematic review of nearly 8,000 patients found the rate of regret to be only 1% (Bustos, 2021; Garg, 2021 ).
It’s also important to discuss fertility with your doctor ahead of time. If there’s a chance you may want the option of having biological children but still want to have sex organ removal during your surgery, you can consider fertility preservation options (like freezing your sperm or egg freezing ) (Garg, 2021; WPATH, 2012).
Access to care providers
Gender-affirming surgery is becoming increasingly common, but unfortunately, few providers around the country have the skills and sensitivity to manage transgender care (Mani, 2021). If you have to travel out of town to seek gender-affirming surgery, it can be a good idea to try to find any care providers in your local area who specialize in transgender health issues to help guide your follow-up care if need be.
Hidden costs
Hidden costs are another major issue for transgender individuals seeking to transition with surgery. Certain hormone treatments, sperm and embryo freezing, and surgeries can be prohibitively expensive if insurance does not cover any part of the cost. Distance from trained providers can also be an issue; few surgeons are experienced in gender reassignment surgery, so seeing them can be costly and time-intensive (WPATH, 2012).
Gender reassignment surgery can be complex and overwhelming. There is a lot of information out there and many options to consider. But by taking it one step at a time and seeking support from family, friends, and community support groups, it can be an invaluable step in helping a transgender person live in a way that is true to who they are.
If you have any medical questions or concerns, please talk to your healthcare provider. The articles on Health Guide are underpinned by peer-reviewed research and information drawn from medical societies and governmental agencies. However, they are not a substitute for professional medical advice, diagnosis, or treatment.
Ascha, M., Massie, J. P., Morrison, S. D., Crane, C. N., & Chen, M. L. (2018). Outcomes of single stage phalloplasty by pedicled anterolateral thigh flap versus radial forearm free flap in gender confirming surgery. Journal of Urology, 199 (1):206-214. doi: 10.1016/j.juro.2017.07.084. Retrieved from https://pubmed.ncbi.nlm.nih.gov/28765066/
Baker, K. E. (2017). The future of transgender coverage. The New England Journal of Medicine, 11 ;376(19):1801-1804. doi: 10.1056/NEJMp1702427. Retrieved from https://www.academia.edu/40998867/The_Future_of_Transgender_Coverage
Bekeny, J. C., Zolper, E. G., Fan, K. L., & Del Corral, G. (2020). Breast augmentation for transfeminine patients: methods, complications, and outcomes. Gland Surgery , 9 (3), 788–796. doi: 10.21037/gs.2020.03.18. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7347817/
Bustos, V. P., Bustos, S. S., Mascaro, A., Del Corral, G., Forte, A. J., Ciudad, P., et. al. (2021). Regret after gender-affirmation surgery: a systematic review and meta-analysis of prevalence. Plastic and Reconstructive Surgery. Global Open , 9 (3), e3477. doi: 10.1097/GOX.0000000000003477. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8099405/
Bustos, S. S., Kuruoglu, D., Yan, M., Bustos, V. P., Forte, A. J., Ciudad, P., et. al. (2021). Nipple-areola complex reconstruction in transgender patients undergoing mastectomy with free nipple grafts: a systematic review of techniques and outcomes. Annals of Translational Medicine , 9 (7), 612. doi: 10.21037/atm-20-4522 . Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8105810/
Carter, E. E., Crane, C. N., & Santucci, R. A. (2020). Established and experimental techniques to improve phalloplasty outcomes/optimization of a hypercomplex surgery. Plastic and Aesthetic Research, 7(33). doi: 10.20517/2347-9264.2020.81. Retrieved from https://parjournal.net/article/view/3527
Chen, M. L., Reyblat, P., Poh, M. M., & Chi, A. C. (2019). Overview of surgical techniques in gender-affirming genital surgery. Translational Andrology and Urology , 8 (3), 191–208. doi: 10.21037/tau.2019.06.19. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6626317/
Cohen, W. A., Sangalang, A. M., Dalena, M. M., Ayyala, H. S., & Keith, J. D. (2019). Navigating insurance policies in the United States for gender-affirming surgery. Plastic and Reconstructive Surgery. Global Open , 7 (12), e2564. doi: 10.1097/GOX.0000000000002564. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7288898/
Fardo, D., Sequeira, C. M., & Pensler, J.M. (2021). Breast augmentation. [Updated Oct 1, 2021]. In: StatPearls [Internet]. Retrieved on Jan. 28, 2022 from https://www.ncbi.nlm.nih.gov/books/NBK482206/
Garg, G., Elshimy, G., & Marwaha, R. (2021). Gender dysphoria. [Updated July 20, 2021]. In: StatPearls [Internet]. Retrieved on Jan. 28, 2022 from https://www.ncbi.nlm.nih.gov/books/NBK532313/
Heston, A. L., Esmonde, N. O., Dugi, D. D., 3rd, & Berli, J. U. (2019). Phalloplasty: techniques and outcomes. Translational Andrology and Urology , 8 (3), 254–265. doi: 10.21037/tau.2019.05.05. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6626313/
Jolly, D., Wu, C. A., Boskey, E. R., Taghinia, A. H., Diamond, D. A., & Ganor, O. (2021). Is clitoral release another term for metoidioplasty? A systematic review and meta-analysis of metoidioplasty surgical technique and outcomes. Sexual Medicine , 9 (1), 100294. doi: 10.1016/j.esxm.2020.100294. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7930881/
Mani, V. R., Valdivieso, S. C., Hanandeh, A., Kalabin, A., Ramcharan, A., & Donaldson, B. (2021). Transgender surgery - knowledge gap among physicians impacting patient care. Current Urology , 15 (1), 68–70. doi: 10.1097/CU9.0000000000000002. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8137065/
Papadopulos, N. A., Ehrenberger, B., Zavlin, D., Lellé, J. D., Henrich, G., Kovacs, L., et. al. (2021). Quality of life and satisfaction in transgender men after phalloplasty in a retrospective study. Annals of Plastic Surgery, 87 (1):91-97. doi: 10.1097/SAP.0000000000002693. Retrieved from https://pubmed.ncbi.nlm.nih.gov/33661220/
Pariser, J. J. & Kim, N. (2019). Transgender vaginoplasty: techniques and outcomes. Translational Andrology and Urology , 8 (3), 241–247. doi: 10.21037/tau.2019.06.03. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6626315/
Santucci, R.A. (2018). Urethral complications after transgender phalloplasty: strategies to treat them and minimize their occurrence. Clinical Anatomy, 31 (2):187-190. doi: 10.1002/ca.23021. Retrieved from https://pubmed.ncbi.nlm.nih.gov/29178533/
Schmitt, W. P., Eichhorn, M. G., & Ford, R. D. (2016). Potential costs of breast augmentation mammaplasty. Journal of Plastic, Reconstructive, & Aesthetic Surgery, 69 (1):55-60. doi: 10.1016/j.bjps.2015.09.012. Retrieved from https://pubmed.ncbi.nlm.nih.gov/26601873/
Van Caenegem, E., Verhaeghe, E., Taes, Y., Wierckx, K., Toye, K., Goemaere, S., et. al. (2013). Long-term evaluation of donor-site morbidity after radial forearm flap phalloplasty for transsexual men. Journal of Sexual Medicine, 10 (6):1644-51. doi: 10.1111/jsm.12121. Retrieved from https://pubmed.ncbi.nlm.nih.gov/23534878/
van de Grift, T. C., Pigot, G. L. S., Kreukels, B. P. C., Bouman, M. B., & Mullender, M. G. (2019). Transmen's experienced sexuality and genital gender-affirming surgery: findings from a clinical follow-up study. Journal of Sex and Marital Therapy, 45 (3):201-205. doi: 10.1080/0092623X.2018.1500405. Retreived from https://www.tandfonline.com/doi/full/10.1080/0092623X.2018.1500405
Wilson, S. C., Morrison, S. D., Anzai, L., Massie, J. P., Poudrier, G., Motosko, C. C., et. al. (2018). Masculinizing top surgery: a systematic review of techniques and outcomes. Annals of Plastic Surgery, 80 (6):679-683. doi: 10.1097/SAP.0000000000001354. Retrieved from https://pubmed.ncbi.nlm.nih.gov/29401125/
World Professional Association for Transgender Health. (2012). Standards of Care for the Health of Transsexual, Transgender, and Gender Nonconforming People [7th Version]. Retrieved from https://www.wpath.org/publications/soc
How we reviewed this article
Every article on Health Guide goes through rigorous fact-checking by our team of medical reviewers. Our reviewers are trained medical professionals who ensure each article contains the most up-to-date information, and that medical details have been correctly interpreted by the writer.
Editorial Guidelines | Medical Review Process
Current version
February 10, 2022
Fact checked by
Steve Silvestro, MD
About the medical reviewer
Dr. Steve Silvestro is a board-certified pediatrician and Associate Director, Clinical Content & Education at Ro.
More articles like this
Sexual Health • 5 MIN READ
What are the benefits of avocado sexually?
Sexual Health • 6 MIN READ
All about the banana benefits for men
Sexual Health • 7 MIN READ
Are there any benefits to semen retention?
4 benefits of pineapple sexually, can garlic benefit your sex life, is the penis a muscle or bone.
Sexual Health • 8 MIN READ
Are pills to increase male sex drive and libido legit?
Sexual Health • 4 MIN READ
Can cinnamon benefit you sexually?
3 sexual benefits of zinc, how long does it take for sperm to regenerate.
Health Conditions
- Breast Cancer
- Cancer Care
- Caregiving for Alzheimer's Disease
- Chronic Kidney Disease
- Chronic Obstructive Pulmonary Disease (COPD)
- Digestive Health
- Heart Health
- Mental Health
- Multiple Sclerosis (MS)
- Rheumatoid Arthritis (RA)
- Sleep Health
- Type 2 Diabetes
- Weight Management
Condition Spotlight
Wellness Topics
- Mental Well-Being
- Sexual Health
- Vitamins and Supplements
- Women's Wellness
Product Reviews
- At-Home Testing
- Men's Health
- Women's Health
Featured Programs
Video Series
- Pill Identifier
- Crohn’s and Ulcerative Colitis Essentials
- Diabetes Nutrition
- High Cholesterol
- Taming Inflammation in Psoriasis
- Taming Inflammation in Psoriatic Arthritis
Newsletters
- Anxiety and Depression
- Nutrition Edition
- Wellness Wire
Lifestyle Quizzes
- Find a Diet
- Find Healthy Snacks
- How Well Do You Sleep?
- Are You a Workaholic?
Health News
- Can 6-6-6 Walking Workout Help You Lose Weight?
- This Couple Lost 118 Pounds Together Without Medication
- 5 Science-Backed Ways to Live a Longer Life
- Morning Coffee May Help You Live Longer
- ‘Weekend Warrior’ Workouts for Your 2025 Fitness Goals
This Just In
- 5 Tips for a Healthy Lifestyle
- How to Disinfect Your House After the Flu
- Best Vegan and Plant-Based Meal Delivery for 2025
- Does Medicare Cover Pneumonia Shots?
- Chromosomes, Genetics, and Your Health
- Best Multivitamins for Women
- Best Multivitamins for Men
- Best CBD Gummies
- Best Online Therapy Services
- Online Therapy That Takes Insurance
- Buy Ozempic Online
- Mounjaro Overview
- Youth in Focus
- Healthy Harvest
- Through an Artist's Eye
- Future of Health
Find Your Bezzy Community
Bezzy communities provide meaningful connections with others living with chronic conditions. Join Bezzy on the web or mobile app.

Follow us on social media
Can't get enough? Connect with us for all things health.
What to Expect from Gender Confirmation Surgery

What is it?
For some, though not all, transgender people, surgery is an important and affirming part of the transition process. It can help alleviate feelings of dysphoria , help align your body with your internal sense of your gender, and make it easier to navigate the world in your gender.
Over the years, the names for these surgeries have evolved. Today, many transgender people prefer to use the term “gender confirmation surgery,” because when we say something like gender “reassignment” or “sex change,” it implies that a person’s gender changes when they have surgery.
As many trans folks have noted, surgery doesn’t change one’s gender — it changes the body in which one experiences that gender.
Here, we break down the different types of surgeries available to transgender people.
Top surgery for people assigned female at birth
During puberty, most folks who were assigned female at birth (AFAB) will develop breast or chest tissue.
Top surgery is a procedure to remove the chest tissue and reconstruct the chest to have more of a masculine appearance.
There are three basic top surgery options for AFAB folks:
Double incision
With this procedure, incisions are typically made at the top and bottom of the pectoral muscle and the chest tissue is removed.
The skin is pulled down and reconnected at the sight of the lower incision.
The nipples are also removed and used to create a graft that has the appearance of a nipple. This method generally results in decreased nipple sensation.
With the Inverted-T and Buttonhole methods, incisions are made around the nipples. This allows them to remain intact and retain sensation.
This procedure may work best for people with medium- to large-sized chests.
Periareolar and keyhole
With the periareolar procedure, one incision is made around the areola, and a larger circular incision is made around that.
The breast tissue is removed, as is the ring of skin between the two incisions.
The skin is then pulled in around the nipple — like a drawstring — and reattached. This leaves the nipple intact.
With the keyhole procedure, there’s only one incision. It goes underneath the nipple, allowing the chest tissue to be removed from there.
These procedures may work best for folks with smaller chests.
Bottom surgery for people assigned female at birth
AFAB folks were, for the most part, born with a vagina and clitoris.
Although testosterone use increases the size of the clitoris, some transmasculine people may wish to have some form of bottom surgery in which the genitals are reconstructed to create a phallus.
Testicular implants may be added, the urethra may be rerouted into the new phallus, and the vagina and other reproductive organs may be removed.
Bottom surgery options for AFAB folks include the following:
Metoidioplasty
The enlarged clitoris is released from the clitoral hood to create a new phallus.
Folks who get this surgery may have their urethra rerouted with a graft from their cheek or the inside of the vaginal wall so they can urinate through the new phallus.
The addition of testicular implants is also possible.
This surgery is only possible for folks who have been on testosterone. It’s a great option for people who want something less invasive than phalloplasty.
Phalloplasty
A graft is taken — typically from the forearm, thigh, or back — and used to create a penis.
Depending on the type of surgery , the urethra may be linked to allow urination through the new penis, and an implant may be installed to allow the penis to become erect.
This surgery is best for people who want a more realistic, average-size penis .
Hysterectomy, oophorectomy, and vaginectomy
AFAB trans people have a number of options when it comes to their reproductive organs. This includes removal of the uterus ( hysterectomy ), removal of one or both ovaries ( oophorectomy ), and removal of the vagina.
Top surgery for folks who were assigned male at birth
For transfeminine people and nonbinary folks who were assigned male at birth (AMAB), the absence of breast tissue can be a source of discomfort or dysphoria.
While hormone therapy can increase the size of the chest, some may wish to have top surgery to increase the size of the breasts, known as breast augmentation.
Breast augmentation
An incision is made along the areola, at the point where the chest and breast tissue meet or under the armpit.
The surgeon then inserts either a custom-sized silicone or saline implant and sutures the incision.
Silicone implants tend to be softer and more realistic. Saline implants are typically less expensive.
This surgery is great for anyone who wants to have a larger chest.
Bottom surgery for people who were assigned male at birth
Most AMAB folks have a penis and testicles. For transfeminine and nonbinary AMAB folks, this may be a source of discomfort which bottom surgery can relieve.
There are three basic bottom surgery options for AMAB folks:
Vaginoplasty
A functioning vagina is created out of existing tissue . The most common method is through penile inversion. The penis is inverted to create a vagina, the tip of the penis becomes a functioning clitoris, and the scrotal skin becomes the labia.
There are variations in which a graft from the intestine is used to create the vaginal wall (to supply more lubrication), or in which the scrotum is inverted to create a vaginal wall.
This surgery may be an option for anyone who wishes to have a functioning vagina.
Orchiectomy and scrotectomy
With these procedures, one or both testicles or the entire scrotum are removed.
Orchiectomy is a relatively inexpensive option in which the testes are removed. This allows your body to create less endogenous testosterone, which can be especially helpful for those on hormone replacement therapy.
Scrotectomy offers similar results, but it isn’t recommended for folks who wish to have a vaginoplasty. Scrotal skin is required for a vaginoplasty.
Things to consider
The increasing availability of gender confirmation surgeries is an incredible mark of progress for the transgender community. However, it’s important to note a few things about gender confirmation surgery and whether it’s the right choice for you.
Surgery isn’t the only aspect of medical transition
Representations of trans people tend to focus on the surgical aspects of transition, especially bottom surgery.
However, hormonal transition is also a valid medical option and can often produce results that alleviate dysphoria.
And, remember, medical transition isn’t necessary unless it’s something you truly want.
Surgery isn’t the same for everyone
One of the biggest things to remember is that not everyone wishes to have gender confirmation surgery, and the results — mental, physical, and emotional — will be different for everyone. Do your research and figure out what the right path is for you.
Surgery doesn’t define your experience or make you more valid
Surgery can be incredibly affirming for those who wish to have it.
But it’s important to remember that gender confirmation surgery simply changes the body in which you experience your gender, not your gender itself.
Your gender is valid, regardless of whether you want to have surgery.
Cost and insurance
Section 1557 of the Affordable Care Act (ACA) prohibits discrimination based on gender identity by any public insurance program or private insurance company receiving federal funding.
This means that if you have Medicare, Medicaid, public school insurance, or a private plan through the ACA marketplace, it’s illegal for you to be discriminated against for being transgender.
Your insurance may cover gender confirmation surgery in order to avoid breaching this non-discrimination clause. However, the law doesn’t require that an insurance company cover any specific procedures, leaving it somewhat open to interpretation.
Recent news from the White House makes it unclear how insurance companies will handle gender confirmation surgeries in the future. But as it currently stands, many people are able to get their surgeries covered by insurance.
If you don’t have insurance or if your insurance won’t cover your surgery, you may need to raise the funds yourself and pay out-of-pocket. Many trans people have used crowdfunding or medical loans to cover their surgeries.
Regardless, these are the prices you can expect to pay for the surgeries we’ve listed here.
- Transmasculine top surgery: Ranges from $3,000 to $11,000, depending on surgery type and surgeon.
- Transmasculine bottom surgery: Starts around $4,000 for metoidioplasty and goes up to $22,000 for phalloplasty.
- Transfeminine top surgery: Ranges from $3,000 to $11,000 , depending on surgeon and location.
- Transfeminine bottom surgery: Starts around $4,000 for orchiectomy and goes up to $20,000 for vaginoplasty.
How to find a provider
Depending on your insurance coverage, you may need to find someone in your network. You can check with your insurance company to see which surgeons are in your network.
If you don’t have insurance or your insurance won’t cover your surgery, you may be able to select a doctor you like based on their work and other factors.
These are a few great resources for finding a provider:
- Metoidioplasty.net
- MTF Surgery
- Topsurgery.net
- Trans HealthCare
- TS Surgery Guide
The bottom line
Gender confirmation surgery certainly isn’t the right choice for everyone.
But for the folks who want — and in fact need — confirmation surgery, it can be an incredible opportunity to help align your body with your internal sense of self.
If gender confirmation surgery is in your future, be sure to do your research to find the right surgeon for you.
KC Clements is a queer, nonbinary writer based in Brooklyn, NY. Their work deals with queer and trans identity, sex and sexuality, health and wellness from a body positive standpoint, and much more. You can keep up with them by visiting their website , or by finding them on Instagram and Twitter .
How we reviewed this article:
- Bluebond-Langner R, et al. (2017).Top surgery in transgender men: how far can you push the envelope? DOI: https://journals.lww.com/plasreconsurg/Fulltext/2017/04000/Top_Surgery_in_Transgender_Men___How_Far_Can_You.14.aspx
- Female-to-male price list. (2018). http://www.thetransgendercenter.com/index.php/femaletomale1/ftm-price-list.html
- Frey J, et al. (2016). Asystematic review of metoidioplasty and radial forearm flap phalloplasty infemale-to-male transgender genital reconstruction: is the “ideal” neophallus anachievable goal? DOI: https://dx.doi.org/10.1097%2FGOX.0000000000001131
- Horbach S, et al. (2015). Outcomeof vaginoplasty in male‐to‐female transgenders: a systematic review of surgicaltechniques. DOI: https://doi.org/10.1111/jsm.12868
- Male-to-female price list. (2018). http://www.thetransgendercenter.com/index.php/maletofemale1/mtf-price-list.html
- Metoidioplasty cost. (2018). https://www.realself.com/ftm-metoidioplasty/cost
- MTF breast augmentation cost.(2018). https://www.realself.com/mtf-breast-augmentation/cost
- Section 1557 of the Patient Protectionand Affordable Care Act. (2010). Health and human services. https://www.hhs.gov/civil-rights/for-individuals/section-1557/index.html
- Stojanovic B, et al. (2017).One-stage gender confirmation surgery as a viable surgical procedure forfemale-to-male transsexuals. DOI: https://doi.org/10.1016/j.jsxm.2017.03.256
- Weigert R, et al. (2013). Patientsatisfaction with breasts and psychosocial, sexual, and physical well-beingafter breast augmentation in male-to-female transsexuals. DOI: https://journals.lww.com/plasreconsurg/Abstract/2013/12000/Patient_Satisfaction_with_Breasts_and.9.aspx
Share this article
Read this next
What does having a vagina mean? There’s no right or wrong way of having a relationship with your vagina, and yet having or not having one can…
People who are genderqueer often experience their gender as fluid, meaning it can shift and change at any given time. Here's what it might look like…
We created an LGBTQIA+ safer sex guide that understands the true complexity and diversity across gender identities, sexual orientation, attractions…
You may have heard the term “misgendering” before, but what exactly does it mean? Here's what you should know about what pronouns to use and when.
Society typically tells us that there are two sexes, male and female, and that they align with two genders, man and woman. With the increased…
You may have heard the term "deadnaming" before, but what exactly does this mean? Here's what you should know and why it matters.
Cissexism is based on the assumption that all people are cisgender. This is so deeply ingrained in our society, so many people say and do things that…
Words can unconsciously undermine transgender and nonbinary people, so being conscious of our words and their affect is so important.
Aspects of social transitioning available to people of any age, but elements of medical transitioning may need to wait until certain prerequisites are…

IMAGES
COMMENTS
Dec 13, 2023 · Gender reassignment is an outdated term for gender affirmation surgery. The new language, “gender affirmation,” is more accurate in terms of what the surgery does (and doesn’t) do. No surgery can reassign your gender — who you know yourself to be.
Gender-affirming surgery (GAS) is a surgical procedure, or series of procedures, that alters a person's physical appearance and sexual characteristics to resemble those associated with their identified gender.
Feminizing surgery, also called gender-affirming surgery, involves procedures that help better align the body with a person's gender identity. Research has found that gender-affirming surgery can have a positive impact on well-being and sexual function.
Apr 3, 2024 · Gender affirming surgeries (GAS) can help a person feel more comfortable and live as their most authentic self. They involve using surgical procedures to change a person’s appearance.
Feminizing Gender-affirming surgery for transgender women or transfeminine non-binary people describes a variety of surgical procedures that alter the body to provide physical traits more comfortable and affirming to an individual's gender identity and overall functioning.
Aug 14, 2024 · For transgender or gender nonconforming people, making changes to their bodies is a way of affirming their identity. A trans person can choose from multiple procedures to...
Oct 7, 2021 · What is Gender Confirmation Surgery? Gender confirmation surgery (GCS), known clinically as genitoplasty, are procedures that surgically confirm a person's gender by altering the genitalia and other physical features to align with their desired physical characteristics. Gender confirmation surgeries are also called gender affirmation procedures.
Feb 10, 2022 · Gender reassignment surgery—also called gender affirmation surgery, sex reassignment surgery, transgender surgery, and gender confirmation surgery—refers to several procedures that change the shape and function of a person’s genitalia (and potentially face and other features) to better align with their gender identity.
Top surgery is surgery that removes or augments breast tissue and reshapes the chest to create a more masculine or feminine appearance for transgender and nonbinary people. Facial gender surgery: While hormone replacement therapy can help achieve gender affirming changes to the face, surgery may help.
Dec 22, 2018 · It can help alleviate feelings of dysphoria, align your body with your internal sense of your gender, and make it easier to navigate the world in your gender. Here’s what to expect.