
An official website of the United States government
Here's how you know
Official websites use .gov A .gov website belongs to an official government organization in the United States.
Secure .gov websites use HTTPS A lock ( Lock Locked padlock ) or https:// means you’ve safely connected to the .gov website. Share sensitive information only on official, secure websites.

MENU Elder Justice Initiative Home
- Physical Abuse
- Psychological Abuse
- Financial Exploitation
- Neglect & Abandonment
- Sexual Abuse
- Red Flags of Elder Abuse
- State Elder Abuse Flyers
- Find Help Near You
- Senior Scam Alert
- Prosecutor Training & Resources
- Federal & State Samples
- State Elder Abuse Statutes
- Law Enforcement
- Victim Specialists
- Network Locator Map
- Highlighted Networks
- MDT Resources
- MDT Webinars
- MDT Guide & Toolkit
- MDT Peer Support Listserv Community
- Guardianship
- Federally Funded Research
- Forensic Research
- Foundational Articles
- Elder Abuse Flyers
- Community Presentations
- Webinars, Training, and Events
Abuse Stories
This collection contains all stories of abuse that have been featured in the Victim, Family & Caregiver Resources: Neglect & Abandonment , Sexual Abuse , Physical Abuse , Psychological Abuse, and Financial Exploitation .
NEGLECT & ABANDONMENT
Abandonment by adult daughter.
Juliette, 87, lived with her daughter, Nanette, for the past 3 years. Nanette helped Juliette with daily activities, such as getting her meals, bathing, and cleaning the house. Nanette decided to move in with her boyfriend in another state and left her mother alone in the home. About a week later, Juliette’s niece happened to be in town and stopped by to visit her aunt. She saw that the inside of the house was in very bad condition and found Juliette in poor health. Juliette’s niece contacted Adult Protective Services (APS) and the State Area Agency on Aging.
Neglect by Daughter and Son-in-Law
Kofi, 84, was diagnosed with Alzheimer’s disease and moved in with his daughter's family. Sometimes Kofi had trouble sleeping, had physical and verbal outbursts, and began wandering. His daughter and son-in-law were afraid that Kofi might wander out of the house if they left him alone. They locked the doors to the house so that Kofi could not get out and wander around when they left for work. A neighbor noticed Kofi trying to get out of the house. She contacted the local police and Adult Protective Services (APS).
Neglect by Son and Daughter-in-Law
Tamara, 76, lived alone but had trouble getting around. Her son and his wife asked Tamara to move in with them. Tamara had her own bedroom on the second floor and stayed there most of the time. She could not use the stairs easily. Her son and daughter-in-law both traveled frequently for work and sometimes neglected to give her adequate food and water. They also failed to groom her or to clean her room consistently. One day Tamara became dizzy, weak and disoriented so her daughter took her to the hospital. The hospital staff discovered that she was dehydrated, disheveled and obviously unwashed. They asked about her care but Tamara said she was well cared for. Nevertheless, as required by law, the hospital staff reported suspected neglect to Adult Protective Services (APS).
Neglect by Sons
Clarence, 79, invited his two adult sons to move in with him so he would not be alone after his wife died. The sons soon sent Clarence out to live in the shed and locked him out of the house. Sometimes his sons put food out for him. Occasionally they gave him a basin of cold water with a washcloth. When one of Clarence’s neighbors noticed that Clarence seemed to be living in the shed, she called Adult Protective Services (APS) anonymously and reported what she had seen. She then decided Clarence may need immediate help so she called the police to do a welfare check.
Abandonment by Guardian/Conservator
Henrietta, 88, required a court appointed guardian due to combined physical and mental disabilities that left her partially incapacitated. Her niece, Roberta, was appointed as Henrietta’s guardian. Roberta visited Henrietta in her home a few times but then never came back and made no further arrangements for her care. A neighbor noticed the lack of activity at Henrietta’s house. The neighbor knocked but couldn’t get Henrietta to answer door so she called law enforcement for a welfare check and Adult Protective Services (APS).
June, 73, suffered a severe brain injury. At first she was able to care for herself but as she got worse, a court appointed Sam as her legal guardian to assist her. He saw June two times in the first six months but did not return to see June and did not arrange for her care. He falsified reports to the court stating that he saw June every three months. As a result, no one knew that June was living on her own without Sam’s help. June was unable to remember to clean her house and the trash had not been taken out in many months. Due to the deterioration of her house, June received a visit from a county health officer who discovered that June was very frail. The county health officer was a mandatory reporter and called Adult Protective Services (APS). APS petitioned the court for a new guardian.
Back to Top
SEXUAL ABUSE
Sexual abuse by nursing aide.
Margaret, 77, lived in a nursing home that was known for good residential care. One day, a nursing aide noticed that Margaret appeared anxious but Margaret would not explain why. While preparing her for a bath, the nursing aide saw multiple bruises on Margaret's arms, neck and back and asked what happened. Initially, Margaret did not say anything. Subsequently, the director of nursing learned from another resident that a new aide had sexually assaulted Margaret. As required by law, the director of nursing reported the sexual assault to Adult Protective Services (APS), and APS initiated an investigation, involving the Ombudsman and local law enforcement.
Sexual Assault by Caregiver
Eduardo, 80, had a stroke. His family hired an in-home caregiver to assist with his daily needs such as bathing and going to the toilet. One day his daughter stopped by to help see her Dad. As she helped him get dressed, he winced and she noticed that his genital area was red and irritated. Her father started to cry and mumbled something about the caregiver hurting him there. The daughter immediately called Adult Protective Services (APS) to make a report. She also called the agency where the caregiver worked, made a complaint, and ended services. APS alerted the law enforcement.
Sexual Assault by Family Member
Pearl, 70, took her nephew in when his mother could not handle his behavior problems. The nephew began viewing pornography on the TV that he shared with his aunt. Pearl was uncomfortable about this and told her nephew to stop. One day, the nephew came home and was high on drugs. He forced himself sexually upon his aunt. Pearl called 911 for local law enforcement and went to the hospital where she met with a sexual assault victim specialist.
Sexual Abuse by Guardian/Conservator
Angela, 71, required guardianship because of her continued alcohol and drug abuse. The court appointed Richard as her guardian. Soon after his appointment, he gave Angela more drugs, sexually assaulted her, and threatened her with prison for her drug use if she reported him. Angela summoned the courage to go the local police and contacted a lawyer to obtain a new guardian.
PHYSICAL ABUSE
Physical abuse by adult grandsons.
Katherine, 82, raised two grandsons, Joel and Kent. They had physically abused her since they were teenagers. After 12 years in prison, Joel returned to his grandmother's home because he had nowhere to go. One night Joel came home and was drunk. He banged on the door but Katherine told Joel to go away. After he entered the house through a back window, Joel beat his grandmother. Katherine went to a neighbor’s house and called 911. Joel was arrested and Katherine was taken to the hospital. The police contacted Adult Protective Services (APS).
Physical Abuse by Disabled Adult Son
When George, 79, lost his wife of 50 years to cancer, his son, Lawrence, came to live with him. Lawrence was on disability due to a traumatic brain injury. The brain injury caused behavior changes, including difficulty with self-control and verbal and physical outbursts. The injury also caused violent mood swings. Occasionally, Lawrence went to a neighbor's apartment and got drunk. One night when Lawrence returned home, George asked him if he was drunk. Lawrence yelled "NO" and punched his father in the face. Because George was afraid of further violence, he called 911 to get help from the police.
Physical Abuse by Spouse
After 58 years of marriage, Virgil and Ella, both 83, knew each other's habits well. Sometimes, when they argued they became physically violent. Nevertheless, they said they loved each other and had never considered divorce. Violence was unfortunately a part of their relationship. As Ella aged, she developed osteoporosis. She began to worry that if she fell down when they were fighting each other she might end up with a broken bone. She confided this to a friend, and her friend suggested calling the local domestic violence hotline to speak with a counselor.
Physical Abuse by Guardian/Conservator
Blair, 65, had no close relatives. Because of early-onset dementia, he was placed in a nursing home and required guardianship. Chris, Blair’s guardian, came to Blair’s nursing home every few months to see how Blair was doing. During the last visit, Chris began slapping Blair to wake him up. Joan, a care attendant rushed to the room when Blair began crying out for Chris to stop. Joan noticed marks on Blair’s face and asked what had happened. Blair was unable to tell Joan what had happened but Chris quickly left the room. Joan reported the incident to her supervisors who helped her make a report to Adult Protective Services (APS). The report triggered involvement by the state ombudsman and local law enforcement.
Physical Abuse by Long-Term Care Aide
Monica, 79, was placed in a long term care facility when her ALS became severe and her family could no longer care for her. Her family became concerned when they saw bruising on her arms and back. Monica was not able to speak and could not tell her family how she got the bruises. Monica’s family asked the staff about the bruising but was not satisfied with the explanation. The family also noticed that when a certain aide helped bathe her, Monica became upset and agitated. They suspected that the aide was hitting Monica and called local law enforcement.
PSYCHOLOGICAL ABUSE
Psychological abuse by daughter.
Zoe, 79, was healthy, independent and lived with her unmarried daughter, Trish, to share expenses. Zoe believed they had a good relationship. Nevertheless, Trish sometimes yelled at Zoe, calling her horrible names and telling her she was worthless. Trish began threatening to put Zoe in a nursing home. Zoe tried to ignore these rants because she was grateful to live with her daughter. However, she thought she deserved to be safe from such comments. Zoe eventually told a close friend about Trish’s yelling and threats. The friend suggested that Trish and Zoe seek counseling and that Trish get respite help from a local Agency on Aging.
Psychological and Physical Abuse by Spouse
Sarah, 75, had been married for over 50 years to Saul who was abusive. The abuse had a pattern. Her husband would start following her around watching her every move. Then he would make comments under his breath. Finally, he would start pointing his finger in her face and pushing her around. Since Saul’s retirement, this pattern seemed to be getting worse and happening more often. Sarah picked up a pamphlet on Domestic Violence at her synagogue and decided to make her first call for help. From her conversation with the domestic violence advocate, she learned about resources in her area and steps she could take to be safe.
Jane had not seen her friend Harry, 87, at Mass for weeks. This was not like her friend since Harry went to Mass almost every Sunday. Jane stopped by Harry’s house. Harry answered the door and Jane was shocked. Her friend had lost weight, looked terrible, and had obviously been crying. Harry told Jane in a hushed voice that since his daughter had moved in she would not let him go to church, the senior center, or even out of the house. Harry said that his daughter was now controlling everything including his money. Before Jane could say anything, Harry’s daughter started yelling and Harry quickly closed the door. Jane decided to make an anonymous report to Adult Protective Services (APS).
Psychological Abuse by Guardian/Conservator
Mark, 75, had Alzheimer’s disease and was beginning to have severe memory loss and trouble walking around the house. Mark’s paid caregiver, Yolanda, asked the court to appoint a guardian. Each time the guardian, Mrs. McKee, visited with Mark, she made fun of his memory problems and inability to remember where he was or even who Yolanda was. Yolanda became worried about Mark and the fact that Mrs. McKee, the court appointed guardian, did not seem to take Mark’s condition seriously. Yolanda called Adult Protective Services (APS) and the probate court to review Mark’s guardianship.
Psychological Abuse (cyber bullying) by Stranger
Rosie, 75, lived alone in an independent senior housing community. Her next door neighbor, a disabled retiree, repeatedly emailed her rude messages and sent vulgar and threatening messages to her cell phone. Fearing her neighbor might harm her if she told him to stop Rosie contacted local law enforcement, and filed criminal charges as well as a petition for a civil restraining order. She also notified housing management.
FINANCIAL EXPLOITATION
Financial Exploitation by Family, Close Friends, or Neighbors
Financial Exploitation (fraud) by Spouse
John, 68, and Bernice, 65, had a “second marriage.” John worked as an engineer and Bernice stayed home. Jointly, they had purchased 22 acres with a second home for their retirement. Trying to mend poor relationships with her sons from her first marriage, Bernice asked John to add one son to the property deed. He agreed. While John was on a business trip, Bernice faxed John the last three pages of the deed for his signature. He signed and returned the form. Unknowingly, he had signed a form deeding the entire property to Bernice who then “gifted” the property to her son. John contacted a lawyer.
Financial Exploitation (identity theft) by Adult Child
Joseph and Malvina, both 80 and retired, had taken in their daughter after her release from prison. Soon after she moved in, the couple received one credit card bill for $8,347, another for $12,694, and a third for $10,012. The couple had no idea their daughter had used their credit cards or that she had opened additional credit card accounts in her mother’s name. Now, Joseph and Malvina were faced with significant debt. The couple’s other adult child contacted Adult Protective Services (APS), the credit card company and the Federal Trade Commission (FTC).
Financial Exploitation (theft) by Guardian/Conservator
Monte, 82, had moderate dementia and required guardianship due to his worsening disease. Unfortunately, Monte had never given his only son, Samson, Power of Attorney. Monte also no longer had sufficient mental capacity to execute a power of attorney for Samson, who now lived out of state. Monte’s personal assistant, John, handled all of Monte’s financial transactions for him. Samson was concerned about John’s access to his father’s finances and reviewed Monte’s account statements while visiting his father over the summer. Samson discovered that several times John had taken over $3000 from one of Monte’s little used accounts. Samson contacted the investment firm, local law enforcement and Adult Protective Services (APS) for help.
Financial Exploitation (misuse of a power of attorney) by Relative
Russell, 88, needed help managing his day to day affairs. His nephew, Jack was out of work and offered to come and live with Russell and help him while Jack looked for a job. Jack took his uncle to the bank saying he wanted to protect Russell’s money. Russell told the bank teller to add Jack to his bank accounts. Jack then downloaded a power of attorney (POA) form from the Internet and had Russell sign it. With the POA, Russell’s credit card company added Jack as a second user to his credit card. When Russell's sister visited him, she asked about the situation. Russell told her that he thought their nephew was stealing his money. She and Russell went to the bank and learned that Jack had spent a considerable amount of his uncle’s money. The sister alerted bank officials, Adult Protective Services (APS) and local law enforcement. Russell filed for an emergency civil protective order to have Jack removed from his home.
Financial Exploitation (theft) by Friend
Ya, 84, became friends with Michelle, 72, in a computer class at the senior center. Using her own computer, Michelle established an online account to help Ya pay her bills. However, Michelle wrote checks for some of her own bills as well as for Ya’s bills. Ya was unaware that Michelle was writing checks for herself until she saw a returned check made out to a cell phone company. Ya didn’t own a cell phone. When she checked her account, Ya discovered that most of her money was gone. Ya contacted local law enforcement and asked her bank to investigate.
Financial Exploitation (promises exchanged) by Acquaintance
Barbara, 76, a retired high-ranking federal government employee, was independent and lived alone. She was recently diagnosed with Alzheimer’s disease and knew she would need more help in the future. Barbara asked Margie, a former neighbor, who was recently divorced, to move in with her. Over time, they agreed that Margie would care for Barbara in her old age and that in return, Barbara would provide Margie’s with food and housing. Barbara gave Margie her power of attorney for access to all her accounts and named her the sole beneficiary of her investment portfolio. After a several months, Barbara noticed her accounts were almost empty and called local law enforcement which also notified Adult Protective Services (APS).
Financial Exploitation by Trusted Professionals
Financial Exploitation (inappropriate products) by Investment Broker
Jackie was a successful investment broker. She had a reputation for making her clients wealthy. Recently Julio, 80, asked Jackie for financial advice. She recommended investments that had high growth potential but were risky for older adults. When Julio’s daughter reviewed his investment portfolio, she found he had investments that wouldn’t provide a return for 30 years and would do Julio little good. Julio contacted the Commodity Futures Trading Commission (CFTC) to check the background of financial professionals, the Securities and Exchange Commission ( SEC) and Adult Protective Services (APS).
Financial Exploitation (investment fraud) by Financial Advisor
Millie, 63, was a public school cafeteria worker who saved for retirement and wanted to help her grandson go to college. A friend recommended Tom, a polite, outgoing financial adviser. Millie didn’t understand the stock market but, after attending a retirement seminar, trusted Tom to invest her money. When she wanted to give her grandson money for college, Millie learned most of the money she had invested was gone. Tom had created fake account statements that showed Millie was making money. Millie contacted Tom’s company and reported him to the Attorney General and Adult Protective Services (APS) in her state.
Financial Exploitation (investment fraud) by Tax Preparer
Alex, an accountant, gave discounts for tax preparation to clients who were over age 65. He built a clientele of wealthy older single adults, widows or widowers, and found ways to get them tax refunds. Many of Alex’s clients gave him Power of Attorney; he also served as their financial adviser. Upon request, Alex gave his clients a statement of their account. Otherwise, he called clients with good news about their investments or about tax loopholes that he took advantage of for the client. When a client’s son learned the deed to his father’s house was in Alex’s name, he looked into his father’s finances and discovered Alex controlled all of his father’s assets. The client’s son contacted the Attorney General, IRS and Adult Protective Services (APS) in his father’s state.
Financial Exploitation (forgery) by Professional Caregiver
Amarjit, 91, paid his own bills. When he opened his bank statement he noticed four $150 checks had been made out to his home health aide. He knew he had not written or signed the checks. Amarjit contacted his bank and local law enforcement.
Financial Exploitation (improperly obtained power of attorney) by Professional Caregiver
Roman, 84, was bedridden. He hired Bob to provide caregiving services. Soon after, Bob forged Roman’s signature to create a fake Power of Attorney (POA) that gave Bob the power to act in Roman’s place. Using this illegal Power of Attorney, the bank allowed Bob to put his name on Roman’s savings and checking accounts. Bob explained to the bank that Roman agreed to the change but couldn’t be present because he was bedridden. Bob later put his own home address name on Roman’s accounts. Roman became concerned when he stopped receiving monthly statements from the bank. Roman contacted the bank immediately and local law enforcement.
Financial Exploitation (fraud) by Representative Payee
Carollee appeared to take good care of the older adults, including veterans, who lived in the group home where she worked. Because most of the residents were disabled and had no family to represent them, Carollee became the representative payee for their Social Security and Veteran’s Benefits. The regular postal carrier became curious when he started delivering over 30 envelopes from Social Security and Veteran’s Benefits to Carollee’s home each month. He thought she lived alone so he notified the local postal inspector through the US Postal Inspection Service hotline, Veterans Affairs, and Adult Protective Services (APS).
Financial Exploitation (inappropriate product) by Mortgage Broker
John, 68, wanted to provide for his wife, Vickie, 62, and leave money for his children when he died. He and his wife thought their home would provide this economic security after they both retired. Less than a year after his retirement, John had a massive stroke and died. Vickie contacted a mortgage broker whose ad she saw in a local magazine. The mortgage broker persuaded Vickie, who had been diagnosed with dementia, to sign a reverse mortgage on her house. Vickie’s daughter learned of the transaction and contacted local law enforcement and Vickie’s mortgage lender.
Financial Exploitation by Strangers
Financial Exploitation (internet identity theft) by Stranger
Naira, 71, was single, disabled and retired. When she got an email from her bank requesting verification of her account numbers, Naira complied. Later she opened an email that she thought was from a government official investigating Medicare fraud. The email asked her to provide her Medicare number to verify that there was no fraud on her account. When her bank manager called to confirm that she wanted to close her accounts, Naira learned the money in her savings and checking accounts was gone. She told the bank manager about the bank email and he told her that it must have been a scam. When she explained how she’d given her Medicare number after the second email, the bank manager contacted the Centers for Medicaid and Medicare, the Federal Bureau of Investigation and Adult Protective Services (APS).
Financial Exploitation (fraud) by New Sweetheart
Arturo was a popular hair stylist. He was charming and attentive to widows and older women and often asked clients who seemed well-off out to dinner. During these meals, Arturo discussed his financial woes. Some customers gave him their bank account information and put him on their accounts “just in case.” Arturo helped three of these wealthy women manage their real estate investments. Two of them even made him a joint owner of their homes. When one customer died, the executor discovered her bank and investment accounts were depleted, her home now belonged to Arturo, and heirlooms were missing. The executor contacted Adult Protective Services (APS), local law enforcement and the FBI.
Financial Exploitation (grandparent scam) by Stranger
Charlie, 82, received a phone call from a “sheriff” in New Orleans. He said Charlie’s grandson had been arrested for intoxication. To be released, the sheriff said that someone needed to pay the grandson’s fine and that his parents were not home. The sheriff told Charlie to wire money to an online address. After the money was delivered, Charlie got a call from someone he thought was his grandson saying that he needed money to get home from New Orleans. Charlie became suspicious when he asked the person claiming to be his grandson a few personal questions that he couldn’t answer. The call ended amicably. Then Charlie called a nearby Federal Bureau of Investigation field office to report the incident and filed a complaint with the FBI’s Internet Crime Complaint Center online.
Financial Exploitation (home repair scam) by Stranger
At 83, Shirley, who was a retired lawyer now lived alone after the death of her husband. It had become difficult to keep up repairs on her house. One day a handyman she’d never seen before rang her doorbell and told her the gutters on her house needed to be cleaned and that she might need a new roof. Because she didn’t have anyone else to help her with these tasks, Shirley paid him $500 to clean the gutters and an additional $10,000 as a down payment for a new roof. She never saw the handyman again. She told a neighbor what had happened and the neighbor contacted Adult Protective Services (APS), local law enforcement, and the state’s consumer protection agency within the Attorney General’s office.
Financial Exploitation (lottery scam) by Stranger
Armando, 78, was thrilled when someone from the lottery called to confirm he had won $10,000. The person on the phone said that they would send the money after Armando sent a winner's fee of $500. Thinking only about what he would do with the winnings, he wired the $500 “winner’s fee” to the address the caller provided. Because he did not receive the promised lottery winnings after a month, he contacted the Federal Trade Commission (FTC).
Protecting Our Seniors From Abuse & Neglect

Recent Elder Abuse in Nursing Homes: Case Studies
Elder abuse is far more common than many people would like to believe. Help keep your loved one safe by reading these recent case studies on elder abuse in nursing homes. Accepting that elder abuse is a real problem is the first step in preventing it.
Examples of Elder Abuse in Nursing Homes: A Nationwide Problem
Nursing home abuse happens when trust is violated through an act — or a failure to act — that harms a resident. It can include emotional, financial, physical, or sexual abuse as well as nursing home neglect.
Tragically, a 2020 report from the World Health Organization (WHO) estimates that roughly 1 in 6 adults 60 years old and over were the victims of elder abuse in nursing homes and other community settings.
Even worse, WHO warns that this already alarming figure is likely to be too low since only 1 in 24 cases of elder abuse is ever reported.
Recent case studies on elder abuse in nursing homes show that this is, unfortunately, a nationwide problem.
The most common forms of nursing home abuse are:
- Emotional abuse : When an older person is yelled at, threatened, or belittled
- Nursing home neglect : Substandard care of a nursing home resident
- Physical abuse : Any form of violence that leaves an older person significantly injured, including cases of wrongful death
- Sexual abuse : Any sexual contact with an older adult who cannot give their consent
Thankfully, help is available if you or a loved one suffered nursing home abuse or neglect. Get a free case review to see if you can access legal compensation.
Fight back against nursing home abuse and neglect — start now with a free case review.

Examples of Case Studies on Elder & Nursing Home Abuse
1. suspected nursing home abuse in massachusetts.
After hundreds of 911 calls were made about suspected nursing home abuse, a criminal investigation was launched against an assisted living facility in Watertown.
Several of the heartbreaking reports include:
- After responding to a call about a faulty ventilator, firefighters found that none of the electrical outlets in a resident’s room were working
- An injured nursing home resident was on the floor asking for help, but when firefighters asked the staff member in charge about it, she just laughed
- Firefighters found staff performing CPR on a man who had already been dead for hours
Further, in a case of suspected physical abuse at the same nursing home, the daughter of a dementia patient found her mother’s face severely battered.
“It was horrific. She had a huge gash on her forehead and a lump the size of a golf ball, her whole face was bruised.” – Daughter of Massachusetts nursing home resident
These examples reveal a widespread pattern of abuse and neglect by staff, which will hopefully be corrected. No nursing home resident should ever have to endure these hardships.
For many families, filing a Massachusetts nursing home lawsuit is a path to getting the justice and compensation they deserve.
2. Nursing Home Sexual Abuse in Minnesota
A male caregiver at a Minneapolis care facility was sentenced to eight years in prison for the rape of a nursing home resident with Alzheimer’s disease.
“My final memories of my mother’s life now include watching her bang uncontrollably on her private parts for days after the rape, with tears rolling down her eyes, apparently trying to tell me what had been done to her, but unable to speak.” – Daughter of Minnesota sexual abuse victim
A follow-up investigation by CNN revealed that the rapist had assaulted multiple other residents, including those who suffered from mental or physical handicaps, before he was finally caught.
By working with an experienced Minnesota nursing home abuse lawyer , families can hold negligent facilities accountable for allowing such appalling situations to happen. Nursing home lawsuits can help improve care standards and help protect residents in the future.
3. Nursing Home Neglect in Iowa
A nursing home resident in Iowa died after extreme neglect related to dehydration . The emergency room doctor believes she died from a stroke after not receiving any type of fluid for at least 4-5 days . The nursing home was fined $77,463 .
In addition to fines like these that may mean little to a profitable nursing home, families can hold facilities accountable by seeking Iowa nursing home settlements .
In some cases, nursing home lawsuit payouts can reach $1 million or more . These settlements provide justice, financial relief, and help protect other residents by calling attention to severe neglect.
Examples of Elder Abuse in Nursing Homes During the Pandemic
While nursing home abuse and neglect were already a very serious issue, the COVID-19 crisis made things even worse.
Neglect and isolation was responsible for causing severe damage to countless nursing homes residents during the pandemic, according to Human Rights Watch and many other sources.
Nursing home abuse case studies from the COVID-19 pandemic revealed:
- A resident in her 80s who was healthy pre-pandemic died shortly after visitation stopped due to suspected malnutrition.
- In less than a year, a dementia patient living in a nursing home went from 106 pounds to 82 pounds before being discharged and dying several days later.
- A dementia patient in her 70s lost 20 pounds during the pandemic and developed painful bedsores on her buttocks and toes.
While thankfully, the coronavirus is less of an issue in 2024, the impact on nursing homes and their residents won’t soon be forgotten.
Why Does Elder Abuse Happen in Nursing Homes?
Elder abuse in nursing homes is a significant problem that affects residents, their families, and everyone else involved in the abuse.
Here are several main causes of nursing home abuse:
- Inadequate staffing : When staff are stretched to their limit, working long hours without help, it can increase their stress and frustration. For this reason, understaffing can lead to higher rates of abuse.
- Insufficient training: Poorly trained staff are less likely to have the necessary skills to deal with difficult or complex situations, resulting in increased rates of abuse. This is especially true in caring for dementia patients, which requires specialized training.
- Lack of supervision: This occurs when a nursing home operates without a medical director or administrator to properly train and manage staff. Without appropriate leadership in facilities, abuse is more likely to take place.
- Staff burnout: It’s the responsibility of every nursing home to manage the morale of the staff who work for them. When morale is low, staff get frustrated, burned out, and are more likely to commit abuse.
No matter the cause of the abuse, it’s important to know that it’s never acceptable . Every resident deserves to be treated with dignity and respect, and all types of nursing home abuse should be reported.

How Common Is Elder Abuse?
About 16% of nursing home residents report being abused according to a study by the National Library of Medicine.
It is believed that elder abuse is more likely to occur with nursing home residents than with older adults living in community settings. In fact, 2 in 3 nursing home staff members admitted to abusing or neglecting residents in the 2020 WHO report.
In 2023, 94,499 health citations were issued to nursing homes throughout the United States. Of these, 7,654 were directly related to the abuse, neglect, or exploitation of residents.
Common Signs of Nursing Home Abuse
The most common signs of nursing home abuse are physical symptoms and changes in behavior. However, different types of abuse are likely to show different signs.
Some common signs of nursing home abuse and neglect include:
- Bedsores, malnutrition, dehydration
- Bruising, scars, cuts, and welts on the body
- Mumbling, rocking, sucking one’s thumb
- Unexplained STDs or bruising on the genitals
If you witness nursing home abuse or notice signs of it, remember to report it to the proper authorities. For anyone who’s been abused in a nursing home, know that help is available.
Get Help for Elder Abuse in Nursing Homes
If you or a loved one was the victim of nursing home abuse, you may be entitled to compensation. Money awarded in a nursing home lawsuit can help pay for medical expenses and bring peace of mind, knowing that justice was served.
The Nursing Home Abuse Center is dedicated to helping victims of nursing home neglect, abuse, and wrongful death. Contact us now to find out if we can help you and your family.

The Nursing Home Abuse Center (NHAC) was founded to bring justice to those affected by nursing home and elder abuse. Our mission is to educate and empower victims of abuse and their families to take a stand against this unlawful mistreatment. We work to return dignity back to those who have been broken down by nursing home abuse and neglect.
- BMC Health Services Research. (2020). Elder abuse and neglect: An overlooked patient safety issue. A focus group study of nursing home leaders’ perceptions of elder abuse and neglect. Retrieved November 12, 2024, from https://bmchealthservres.biomedcentral.com/articles/10.1186/s12913-020-5047-4
- Fiandaca, C. (2021). I-Team: Watertown long-term care facility investigated for possible abuse, neglect. CBS Boston. Retrieved November 12, 2024, from https://boston.cbslocal.com/2021/02/12/long-term-care-facility-nursing-home-elder-abuse-investigation/
- Human Rights Watch. (2021). US: Concerns of neglect in nursing homes. Retrieved November 12, 2024, from https://www.hrw.org/news/2021/03/25/us-concerns-neglect-nursing-homes
- Merrilees, A. (2019). ’83 Years Old, Unable To Speak, Unable To Fight Back.’ Daughters share heartbreaking stories of abuse in nursing homes. ABC News. Retrieved November 12, 2024, from https://abcnews.go.com/Politics/83-years-unable-speak-unable-fight-back-daughters/story?id=61504444
- SeniorLiving.org. (September 6, 2024). Elder abuse statistics for 2024. Retrieved November 12, 2024, from https://www.seniorliving.org/research/elder-abuse-statistics/
- World Health Organization. (2021). Elder abuse. Retrieved November 12, 2024, from https://www.who.int/news-room/fact-sheets/detail/elder-abuse
Complete Your CE
Course case studies, external link, this link leads outside of the netce site to:.
While we have selected sites that we believe offer good, reliable information, we are not responsible for the content provided. Furthermore, these links do not constitute an endorsement of these organizations or their programs by NetCE, and none should be inferred.
Elder Abuse: Cultural Contexts and Implications
Course #97824 - $30-
#97824: Elder Abuse: Cultural Contexts and Implications
Your certificate(s) of completion have been emailed to
- Back to Course Home
- Review the course material online or in print.
- Complete the course evaluation.
- Review your Transcript to view and print your Certificate of Completion. Your date of completion will be the date (Pacific Time) the course was electronically submitted for credit, with no exceptions. Partial credit is not available.
CASE STUDY 1
For several weeks, church members noticed that Mr. L, 82 years of age, had bruises, cuts, and scrapes on his face, hands, and arms. Mr. L always had some plausible explanation and, knowing that he was the sole caretaker for his very ill wife of 61 years, they did not press the issue. A hospital social worker finally contacted APS after Mr. L drove himself to the hospital emergency room, over 20 miles from his home, with multiple fractures to his left arm. The APS social worker eventually discovered that Mr. L was being attacked by his wife, who was suffering from undiagnosed Alzheimer disease and had become combative. Mr. L did not know that his wife's behavior was a part of her illness and was protecting her.
CASE STUDY 2
Mrs. J, a long time insulin-dependent diabetic, was admitted to the hospital after being brought to her physician's office by a neighbor who became concerned after not seeing Mrs. J for several days. Mrs. J finally told hospital staff members that she had run out of insulin several days ago and had given her grandson all the money she had to go and refill her prescription. He did not return, and Mrs. J did not call family members because she did not want to get him in trouble.
CASE STUDY 3
Mr. B, 74 years of age, complains with increasing frequency of pain. His physician is puzzled by the complaints because the methadone she has prescribed should be controlling the pain. She has already increased the dosage a couple of times and is reluctant to do so again. She finally asked a family member to bring in all of Mr. B's medications so that she could check for drug/drug interactions or perhaps prescribe another medication. Examination of the methadone tablets revealed that someone had switched most of the methadone with over-the-counter potassium tablets, which are nearly the same size and color. Mr. B's failing eyesight prevented him from being able to tell the difference between the very similar tablets. Questioning revealed that Mr. B's niece, a former drug addict, had been living with him in exchange for his care, and that she prepared his medications each day. The family suspected that she was using drugs again, but was reluctant to probe too deeply because there was no one else to care for Mr. B.
CASE STUDY 4
Mr. R, 54 years of age, and Mrs. R, 49 years of age, work full time in very demanding jobs. About one year ago, Mr. and Mrs. R built an apartment addition onto their home, depleting their savings, to accommodate Mrs. R's mother, Mrs. D. Mrs. R is the oldest of three siblings and care for her aging mother had become primarily her responsibility. The 90-minute drive to her mother's apartment in a nearby city each weekend had become increasingly taxing, and her mother's care had become more time consuming. When Mrs. D's long-time physician announced his intent to leave private practice, it became reasonable to make the move. Mrs. D, while not enthusiastic, was agreeable. Mrs. R's brother and sister, who rarely visited or helped with her mother's growing needs, became angry about the move and stated that they had no intention of making such a trip. Now, in addition to working 9 to 10 hours per day, Mrs. R goes home to find numerous messages from her mother with various requests and demands. Additionally, because her mother can see her car drive up, the phone is usually ringing by the time she gets into the house to begin dinner for the three of them. There is an in-home aide who comes three days per week to help with bathing and light cleaning, but lately Mrs. R has questioned whether this is worth the added burden of mediating disputes between the aide and her mother. Each morning before work, Mrs. R prepares her mother's medications for the day and makes sure she has something available for breakfast. She longs for a vacation, but the routine continues seven days per week. Besides, all her vacation and sick leave must be devoted to taking care of her mother's medical appointments and treatments. Lately, Mrs. R has been having difficulty sleeping with disturbing dreams of having forgotten some major task. She feels tired all of the time. She has also noticed that she snaps at her spouse and friends often and that her anxiety level is increasing. Her own household chores are piling up because she does not have the time or energy to do them. Last week she noticed a red rash on her thigh and wonders when she might find the time to see her own doctor.
CASE STUDY 5
Mr. J had returned to live with his mother, Mrs. J, a widow of ten years, after his wife insisted he leave their house. During this time, he became depressed and started to drink. Mrs. J's neighbors became concerned that Mrs. J had lost a tremendous amount of weight and looked sad and disheveled lately. One day, Mrs. J confided to one of her neighbors that ever since her son returned to live with her, he had been pilfering her Social Security checks. Initially, she noticed that small amounts of money were missing from her pocketbook, but now, Mr. J threatens her both verbally and physically. He would smash and throw china at her until Mrs. J handed her signed Social Security check to him.
- About NetCE
- Do Not Sell My Personal Information
Copyright © 2024 NetCE · Contact Us

- The Aging Process
- Attitudes about Aging
- Creativity and Older Adults
- Death, Dying and Grief
- Elder Abuse
- Falls Prevention
- Intergenerational
- Alzheimer's-Dementia Care
- Challenges and Rewards
- Mental Health
- Sexuality, Intimacy and Aging
- Spirituality and Aging
- Abuse Prevention
- Activites for Person with Dementia
- Basic Resident Care
- Conflict Resolution
- Eating, Feeding and Oral Care
- End-of-Life Care
- Fall Prevention, Safe Lifting and Transferring
- Infection Control
- Mental Health and Older Adults
- Nursing Assistant Skills Training
- Pain Management
- Quality-of-Life Issues
- Resident Rights and Dignity
- Restorative Care
- Featured Films
- On-Demand Films
- Film Reviews

Elder Abuse: Five Case Studies
This video explores the issues of family abuse against an older adult very personally from the point of view of five different victims. Their candor in telling about their situation gives the viewer insight into the ambivalent feeling of older abuse victims as they try to find resolution to their pain. In the context of their struggle we also see the various interventions that can be used to help stop the abuse, including counseling, shelters, supportive services and legal action.
Each of the cases in this video is real – not reenacted – and has been tracked over a period of time.
Viewing Options
- Purchase DVD $189.00
- Purchase DVD (Tax Exempt) $189.00
- Rent DVD $55.00
Watch On-Demand
- 24 Hours $3.99
- 2 Weeks $45.00
- 5 Years $189.00
Terra Nova Films is a 501(c)(3) non-profit dedicated exclusively to the production, distribution, and presentation of films, videos and educational material on aging. Donate Now
- Alzheimer’s-Dementia Care
An official website of the United States government
Official websites use .gov A .gov website belongs to an official government organization in the United States.
Secure .gov websites use HTTPS A lock ( Lock Locked padlock icon ) or https:// means you've safely connected to the .gov website. Share sensitive information only on official, secure websites.
- Publications
- Account settings
- Advanced Search
- Journal List

Elder Abuse: A Comprehensive Overview and Physician-Associated Challenges
Karan patel, sean bunachita, hannah chiu, prakul suresh, urvish k patel.
- Author information
- Article notes
- Copyright and License information
Karan Patel [email protected]
Corresponding author.
Accepted 2021 Apr 8; Collection date 2021 Apr.
This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Elder abuse can present in many forms, including physical abuse, psychological/emotional abuse, sexual abuse, financial abuse, and neglect. Many studies estimate that about 10% of all people over the age of 65 experience some form of abuse. These rates are often higher in long-term care facilities such as nursing homes, despite government regulations aimed toward addressing this issue. Because patients who experience abuse tend to have higher rates of hospitalization and mortality, it is important for physicians to be able to accurately identify cases of abuse. However, many studies have found that healthcare professionals are often undertrained and ill-equipped in diagnosing elder abuse. In this article, we outline tools that may be able to aid healthcare professionals in their diagnoses, such as survey-based methodology and common physical signs of abuse. In addition, we propose evidence-based solutions, including the use of multidisciplinary teams and increased training on the subject, so that healthcare professionals can more easily identify victims of abuse. Essentially, it is our hope that this article further spotlights elder abuse and its challenges, while serving as a guide to healthcare professionals.
Keywords: elder abuse
Introduction and background
The World Health Organization (WHO) defines elder abuse as, “a single, or repeated act, or lack of appropriate action, occurring within any relationship where there is an expectation of trust which causes harm or distress to an older person" [ 1 ]. Unfortunately, elder abuse is prevalent around the world, with studies finding that 10% of all people over the age of 65 experience some form of abuse, with rates still continuing to rise [ 2 , 3 ]. Despite these alarming numbers and trends, it is estimated that only 1 in 14 cases of elder abuse are reported to the correct authorities [ 4 ]. Elder abuse can result in serious psychological and physical consequences for victims. Studies have shown that victims of abuse are almost three times as likely to suffer hospitalizations than their counterparts; victims of abuse have also been shown to have significantly higher mortality rates [ 5 , 6 ]. Physicians and other health care providers are among the few that may have an opportunity to intervene when someone is being abused. While taking a history and conducting a physical exam, physicians may be able to detect signs of subtle underlying abuse that a victim may cover up in a normal setting. However, physicians are often under trained and unconfident in their ability to identify abuse in [ 7 ]. As a result, many preventable cases of elder abuse go unnoticed each year.
Forms of elder abuse
Elder abuse comes in various forms which include: (1) physical abuse, (2) psychological/emotional abuse, (3) sexual abuse, (4) financial abuse, and (5) neglect. Physical abuse is defined as any intentional act that results in harm to a person. Psychological or emotional abuse includes verbal threats, harassment, intimidation, and isolation. Sexual abuse occurs when a victim either is forced into a non-consensual act or is incapable of consenting to such an action. Examples of this include, but are not limited to, rape, forced nudity, and inappropriate touching [ 8 ]. Financial exploitation occurs when the abuser is controlling and misusing the victim’s financial accounts. The misuse can include actions such as changing a will, stealing from bank accounts, and performing financial transactions that are not in the best interest of the victim [ 9 , 10 ]. Finally, neglect pertains to situations in which a caretaker does not adequately fulfill their duties; this includes such actions as not taking an elder to their doctor’s appointments and not assisting them with daily activities they cannot do themselves, such as personal hygiene maintenance [ 8 ]. A study conducted by Acierno et al. found that the most common types of abuse experienced by their sample were financial abuse, neglect, emotional abuse, physical abuse, and sexual abuse, in that order [ 11 ]. Nonetheless, the prevalence of each type of abuse has yet to be fully determined, though some studies argue that neglect is actually the most common form of abuse [ 10 , 12 ]. The lack of a clear answer may be a result of variations in settings and methods between studies. As stated previously, elder abuse, in general, is associated with an increased risk of hospitalization and death. One study found an elevated risk of death in patients who experienced elder mistreatment compared to those who did not (odds ratio: 3.1, 95% confidence interval: 1.4-6.7) [ 6 ]. Another study by Dong et al. found an increased risk of hospitalization (odds ratio: 1.97, 95% confidence interval: 1.33-2.61) among victims of abuse [ 5 ]. One thing to note is that rates of hospitalization vary among the different subcategories of abuse. Psychological abuse and neglect were most associated with increased hospitalization, while financial abuse was ranked lower among abuse-related risk factors [ 5 ].
Abuse in long-term care facilities
Nursing homes and other long-term care facilities are among the places with the highest rates of elder abuse. Widespread concern over this first became apparent in the 1970s when there were almost no federal regulations for these facilities [ 13 ]. In 1986, the Institute of Medicine, at the request of Congress, conducted a study in which they found high rates of abuse and neglect among nursing home residents. In 1987, the Nursing Home Reform Act (NHRA), as part of the Omnibus Budget Reconciliation Act, was passed in order to help ensure the overall well-being of residents through federal regulations. The act included laws such as providing Medicare and Medicaid payments to nursing homes only if they complied with government requirements [ 14 ]. The main commandments set forth by the NHRA were tenfold: residents of nursing homes had “(1) the right to freedom from abuse, mistreatment, and neglect, (2) the right to freedom from physical restraints, (3) the right to privacy, (4) the right to accommodation of medical, physical, psychological, and social needs, (5) the right to participate in resident and family groups, (6) the right to be treated with dignity, (7) the right to exercise self-determination, (8) the right to communicate freely, (9) the right to participate in the review of one's care plan and to be fully informed in advance about any changes in care, treatment, or change of status in the facility, and (10) the right to voice grievances without discrimination or reprisal” [ 14 ].
Despite government efforts, elder abuse in nursing homes continues to remain a major problem [ 15 ]. The main types of abuse in nursing homes are as follows: physical abuse (29%), resident-to-resident abuse (22%), gross neglect (14%), financial abuse (7%), and sexual abuse (7%) [ 16 ]. A study conducted by Hawes et al. found that 40% of the staff in their sample reported committing at least one instance of psychological abuse over a 12-month period. These actions included, but were not limited to, yelling and swearing at residents, inappropriate isolation, and denying food privileges [ 17 ]. Another study found that 50% of the nursing home staff admitted to mistreating older patients, 17% of certified nursing assistants (CNAs) reported pushing, shoving, or grabbing a nursing home resident, 23% of CNAs reported swearing at residents, and 51% reported yelling at residents [ 16 ]. These numbers were significantly higher when residents were interviewed about their own experiences. In a study of over 2000 nursing home residents, 44% said they had been abused and 95% said that they had either themselves been neglected or seen another resident be neglected [ 16 ]. While the actions of abusers should never be justified, and we by no means condone them, they may be partially explained by the fact that nursing home staff and healthcare professionals are overworked and understaffed, which may contribute to their growing frustrations. They may then take these frustrations out on the residents in a stint of misplaced anger [ 18 ]. One study found that up to 90% of nursing homes are understaffed, and one nurse’s aide may have to take care of up to thirty patients at once. This is in spite of recommended guidelines for the nursing aide to resident ratio, which typically ranges from 1:3 to 1:6 [ 15 ]. As a result, nursing home reforms, including hiring more employees, may be a critical step to reduce rampant abuse.
Risk factors for elder abuse
In Table 1 , we list factors that are commonly associated with perpetrators and victims of abuse. While this is by no means an exhaustive list, it may serve as a guide to aid in the diagnosis of elder abuse. One thing of note is that there are studies that have found conflicting results with some common risk factors. For example, while many studies cite co-inhabitance as a risk factor for abuse, a study conducted by Li et al. found that living alone was actually a risk factor for abuse [ 19 ]. Meanwhile, another study by Pérez-Cárceles et al. found that co-inhabitance was a risk factor only if the perpetrator had a mental health disorder [ 20 ]. We cite these studies here to remind readers that risk factors should only serve as a starting point and cannot solely be used to raise clinical suspicion for abuse.
Table 1. Victim and perpetrator risk factors.
Diagnosing elder abuse
It is important for elder abuse to first be accurately detected and diagnosed so that swift action can then be taken to intervene before the patient faces any further mistreatment. Yet, studies have shown that healthcare professionals are often inadequately equipped to identify cases of abuse. A US national survey of Emergency Department physicians found that 74% were uncertain whether elder abuse had been clearly defined and characterized, while 58% of physicians lacked confidence in their ability to correctly identify abuse in elderly patients [ 25 ]. This is an especially vital consideration since symptoms of elder abuse often mimic those found in other medical conditions. For example, burns can be mimicked by contact dermatitis while a bone fracture can be a symptom of osteoporosis [ 26 ]. Thus, it is crucial that healthcare providers are able to accurately differentiate between abuse and other conditions so that the appropriate treatment plan can be established. Below are a number of resources and methods that have been typically used to aid with the diagnosis of elder abuse.
Patient history
An essential first step to identifying elder abuse is to ascertain the patient’s history in order to uncover potential risk factors and signs of current abuse. During this time, the healthcare provider should take note of patterns indicating abuse, such as lack of attendance for follow-up appointments, high frequency of injuries, and failing to promptly treat illness or injury [ 9 ]. It is crucial to interview the patient in a private setting, without any relatives or caregivers present, as the abuser(s) may be among that group. Additionally, it is important that the patient is as honest as possible in their answers, and they may be hesitant to share details of abuse if others are in the room [ 13 ]. Physician trust can be further gained by being sympathetic and nonjudgmental of the patient’s answers [ 13 ]. A number of screening tools have also been developed to supplement the history-taking process. These are generally a series of standardized questions either asked to or completed by the patient and help guide the physician to the next course of action. Three examples of common screening tools are shown next.
Screening tools
Elder abuse suspicion index: The Elder Abuse Suspicion Index (EASI) is a two-minute screening tool that features a questionnaire of six dichotomous yes/no survey items, with five answered by the patient and one answered by the physician. When administered to cognitively intact patients 65 years of age or older, the assessment was found to have a sensitivity of 47% and a specificity of 75% if at least one EASI item was answered “yes” [ 27 ]. The EASI instrument possesses a number of advantages: (1) it can be conducted in a short time span, (2) it has been validated for both the English and French languages, and (3) it has been validated in a primary care setting [ 27 , 28 ]. However, it also contains some limitations: it can only be used for cognitively intact elderly patients seen by primary care physicians and it does not offer an evaluation of patient caregivers [ 29 ].
Elder assessment instrument: The Elder Assessment Instrument (EAI) is a 44-item screening tool that includes evaluations of social habits, medical history, and emotional/psychological neglect in the patient, among other questions. Each question is scored on a Likert scale ranging from 1 (no evidence) to 4 (evidence) [ 30 ]. The questionnaire takes approximately 15 minutes to complete and has a sensitivity of 71% and a specificity of 93% when administered by emergency department nurses [ 28 , 29 ]. A few advantages of the EAI are that it is relatively simple to administer, it has been validated in both the English and Spanish languages, and it has been validated for administration by nurses [ 30 ]. Some drawbacks of the assessment are its lack of an overall scoring system and lack of validation in subcategories [ 31 ].
Older adult psychological abuse measure: A third screening tool is the Older Adult Psychological Abuse Measure (OAPAM). The OAPAM is self-administered and specifically assesses psychological abuse by examining the level of risk in factors including isolation, insensitivity and disrespect, shaming and blaming, and reported threats and intimidation, as well as a category for other trusted risk factors [ 29 ]. In subjects who had already experienced an instance of violence and were found to be cognitively intact (as assessed by the Mini-Mental State Examination, or MMSE), one study found that the OAPAM showed 92% reliability [ 29 , 31 ]. However, the study was limited in that it only included participants located in Chicago, Illinois, so additional validation studies will need to be conducted in other populations.
Physical exam
Following suspected elder abuse, it is imperative to conduct a comprehensive physical examination by a trained healthcare professional to uncover further evidence. The exam should encompass the patient’s entire body with a specific focus on detecting signs of abuse. Some common physical signs of mistreatment include welts, bite marks, fractures, dehydration, sexually transmitted infections, and poor hygiene [ 32 ]. It is also important to observe interactions between the patient and caregiver, looking for signs of anxiety or poor eye contact in the patient [ 9 ]. If possible, any findings should be further investigated and confirmed through laboratory testing. Some indications of abuse that can be detected through lab screening are dehydration, malnutrition, low medication levels, and drug poisoning [ 9 ].
Elder abuse reporting and treatment
Nearly all states, with the exception of New York, have laws stipulating mandatory reporting by healthcare professionals even under merely the suspicion of elder abuse [ 13 ]. This typically entails notifying a government regulatory agency, such as the Adult Protective Services (APS), who would then assign a social worker to investigate claims of elder mistreatment. If the patient is deemed to be in a sufficient cognitive state to make their own decisions, then they are free to decline further aid if they desire [ 32 ]. Should social assistance continue, then subsequent interventions tend to involve the cooperation of many different support systems throughout the community over long time periods [ 13 ]. While physicians often play a critical role in initially detecting elder abuse, they lack the amount of free time required to fully sustain follow-up and treatment alone. Thus, successful care must involve the interplay and coordination of a multidisciplinary team of trained professionals [ 13 ].
The ultimate goal of treating elder abuse is to ensure that every facet of the patient’s well-being is promptly addressed and that further mistreatment is prevented. Physical injuries are the first priority to reduce bodily pain and increase the quality of life [ 9 ]. Thereafter, the team should manage other forms of abuse, such as psychological, social, or financial. This could involve a number of interventions, such as mental health services, home health care, and meal delivery [ 13 ]. In the end, it is up to the discretion of the interprofessional team to determine the optimal treatment plan for each patient’s unique situation.
Despite the legal requirements and resources available for reporting elder abuse, it has still been found to be the least reported type of domestic violence [ 33 ]. Physicians and other healthcare professionals are hesitant to report elder abuse for a myriad of reasons. They may believe that patients would be moving from one unwanted environment to another: that of understaffed and unsatisfactory care facilities [ 34 ]. Another concern for physicians is being sued for malpractice, especially if the physician reports suspected abuse when it is not actually occurring [ 35 ]. Further, elder abuse may not be reported due to a lack of training on how to do so. For example, a survey of Emergency Medical Services (EMS) providers discovered that there was an absence of protocols specific to reporting concerns in vulnerable elderly populations [ 36 ]. Finally, if the abuse is perpetrated by a close relative, health professionals may view the issue as a family matter that they should not intrude upon [ 33 ].
Potential challenges and associated solutions
Elder abuse persists due to the lack of awareness and education made available to key professionals. In order to bridge the gaps in detection and reporting, it is necessary to increase the hours of training on this topic for medical professionals. The majority of physicians reported their training on elder abuse to be not very adequate or not adequate at all, with most reporting no more than 10 hours of training. Additionally, two-thirds of residency programs fail to prioritize formal elder abuse training, and half of the physicians surveyed report having no residency training in elder abuse detection at all [ 4 , 37 ]. Thus, the best strategy to combat the lack of awareness is to emphasize and increase the training that is done in medical residency programs, making the requirement for elder abuse training a part of the curriculum [ 38 ]. It has been demonstrated that physicians who were offered continuing medical education (CME) for elder abuse were less likely to ignore the abuse of their patients as a barrier to reporting [ 4 ].
Furthermore, as mentioned previously, nursing homes show high rates of abuse, with one study of elders in nursing facilities finding that 44% of respondents had been subjected to prior mistreatment [ 39 ]. As with physician training, a key step to preventing elder abuse is to increase the education of nursing home caretakers and staff-members. These onsite training sessions teach caretakers how to utilize assistive equipment and raise awareness through discussing what to expect as individuals age, their mental health, and the specific illnesses of individual residents. A handful of nursing homes also prioritize educating residents and their family members, planning lighthearted activities that remind elders of the rightful treatment they should expect to receive [ 40 ]. Beyond this, many nursing homes purposefully remind residents of their safety in an overt way. They help facilitate a relationship between elders and the local police department and make crime prevention and abuse hotlines readily available for staff and residents. Many also have security systems in place and take the initiative to secure the residents’ valuables [ 40 ]. Collectively, these practices contribute to creating a safer environment.
Additionally, many elders experience little relief or justice after facing financial abuse. This is partly due to the reluctance or inability of the elder to testify - but even if a victim is willing to prosecute, they can experience significant obstacles along the way. These include a high standard of proof for evidence that abuse has occurred, a lack of professional knowledge, and communication difficulties if the patient is cognitive- or speech-impaired [ 41 ]. One strategy to streamline the process of prosecution is to utilize multi-disciplinary teams, which include professionals within the justice system, physicians, nurses, mental health workers, and protective services. Having this array of professionals allows access to resources like neuropsychological testing, medical records, and legal services, which increase the likelihood of the case being reviewed, charged, and successfully prosecuted [ 42 ].
While these solutions have been proven to be effective, there are some limitations to them. Increased training during residency can require multi-disciplinary collaboration and agreement within each individual institution, and redeveloping parts of the curriculum will require thorough planning and execution. This includes spending time to seek out experienced and trustworthy educators for training both physicians and care-teams at nursing homes on the ways that they can identify and handle elder abuse. Additionally, whether it is providing additional education or offering expansive resources to support specific cases of elder abuse, organizations must be prepared to allot the appropriate funds needed to support these types of initiatives. Nevertheless, these challenges can be overcome and should be prioritized for the sake of mitigating elder abuse.
Conclusions
Elder abuse is a complex, multifaceted problem that stems from many underlying issues. Despite government intervention, abuse continues to remain a rampant issue in society with studies showing approximately 10% of people over the age of 65 experiencing some form of abuse. Physicians and other healthcare professionals have a unique opportunity to be able to intervene in such cases but are ill-equipped to do so with the current training they receive. As a result, health care professionals should receive more formal training, either in medical school or during residency, in order to increase their confidence in detecting suspected cases of abuse. Additionally, there are more complex issues at hand, such as fear of violating physician-patient trust and widespread misinformation about reporting cases. While these are far more difficult to address, we must take the first steps in the right direction by educating our health care professionals. As awareness about this issue increases, these secondary barriers may begin to be addressed through increased knowledge and further investigation.
The content published in Cureus is the result of clinical experience and/or research by independent individuals or organizations. Cureus is not responsible for the scientific accuracy or reliability of data or conclusions published herein. All content published within Cureus is intended only for educational, research and reference purposes. Additionally, articles published within Cureus should not be deemed a suitable substitute for the advice of a qualified health care professional. Do not disregard or avoid professional medical advice due to content published within Cureus.
The authors have declared that no competing interests exist.
- 1. Elder abuse. [Mar;2021 ]; https://www.who.int/ageing/projects/elder_abuse/en/. 2021
- 2. Elder abuse and neglect. Council on Scientific Affairs, American Medical Association, Chicago Chicago. JAMA. 1987;257:966–971. [ PubMed ] [ Google Scholar ]
- 3. Elder abuse statistics. [Mar;2021 ]; https://www.nursinghomeabusecenter.com/elder-abuse/statistics/ 2020 22:2021. [ Google Scholar ]
- 4. Primary care physicians and elder abuse: current attitudes and practices. Wagenaar DB, Rosenbaum R, Page C, Herman S. https://pubmed.ncbi.nlm.nih.gov/21178151/ J Am Osteopath Assoc. 2010;110:703–711. [ PubMed ] [ Google Scholar ]
- 5. Elder abuse as a risk factor for hospitalization in older persons. Dong X, Simon MA. JAMA Intern Med. 2013;173:911–917. doi: 10.1001/jamainternmed.2013.238. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 6. The mortality of elder mistreatment. Lachs MS, Williams CS, O'Brien S, Pillemer KA, Charlson ME. JAMA. 1998;280:428–432. doi: 10.1001/jama.280.5.428. [ DOI ] [ PubMed ] [ Google Scholar ]
- 7. Physician screening for elder abuse in the emergency department: a literature review. [Mar;2021 ];Worrilow WM, Barraco RD. https://scholarlyworks.lvhn.org/research-scholars-posters/432/ LVHN Res Sch Progr Poster Sess. 2015 [ Google Scholar ]
- 8. Types and signs of abuse. [Mar;2021 ]; https://www.dshs.wa.gov/altsa/home-and-community-services/types-and-signs-abuse.
- 9. Elder abuse. [Mar;2021 ];Johnson MJ, Fertel H. https://www.ncbi.nlm.nih.gov/books/NBK560883/. 2020 [ Google Scholar ]
- 10. Elder abuse and neglect. [Mar;2021 ]; https://www.helpguide.org/articles/abuse/elder-abuse-and-neglect.htm 2021
- 11. Prevalence and correlates of emotional, physical, sexual, and financial abuse and potential neglect in the United States: the National Elder Mistreatment Study. Acierno R, Hernandez MA, Amstadter AB, Resnick HS, Steve K, Muzzy W, Kilpatrick DG. Am J Public Health. 2010;100:292–297. doi: 10.2105/AJPH.2009.163089. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 12. Types of elder abuse. [Mar;2021 ]; https://www.nursinghomeabusecenter.com/elder-abuse/types/. 2020
- 13. Elder abuse. Lachs MS, Pillemer KA. N Engl J Med. 2015;373:1947–1956. doi: 10.1056/NEJMra1404688. [ DOI ] [ PubMed ] [ Google Scholar ]
- 14. The 1987 nursing home reform act. [Mar;2021 ];Klauber M, Wright B. https://www.aarp.org/home-garden/livable-communities/info-2001/the_1987_nursing_home_reform_act.html 2001
- 15. Facts & statistics. [Mar;2021 ];Parker J. https://nanha.org/resources/facts-statistics/ 2021
- 16. Abuse of residents of long term care facilities. [Mar;2021 ]; https://ncea.acl.gov/NCEA/media/docs/Abuse-of-Residents-of-Long-Term-Care-Facilities-_1.pdf 2012
- 17. Elder abuse in residential long-term care settings: what is known and what information is needed? [Mar;2021 ];Hawes C. https://www.ncbi.nlm.nih.gov/books/NBK98786/ 2003
- 18. Nursing home abuse statistics. [Mar;2021 ]; https://www.nursinghomeabuse.org/nursing-home-abuse/statistics/ 2021
- 19. Prevalence and associated factors of elder mistreatment in a rural community in People's Republic of China: a cross-sectional study. Wu L, Chen H, Hu Y, et al. PLoS One. 2012;7:0. doi: 10.1371/journal.pone.0033857. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 20. Suspicion of elder abuse in South Eastern Spain: the extent and risk factors. Pérez-Cárceles MD, Rubio L, Pereniguez JE, Pérez-Flores D, Osuna E, Luna A. Arch Gerontol Geriatr. 2009;49:132–137. doi: 10.1016/j.archger.2008.06.002. [ DOI ] [ PubMed ] [ Google Scholar ]
- 21. Risk factors for elder mistreatment. [Mar;2021 ];Bonnie R, Wallace R. https://www.ncbi.nlm.nih.gov/books/NBK98788/ 2003
- 22. Caregiving and elder abuse. Kohn R, Verhoek-Oftedahl W. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4961478/ Med Health R I. 2011;94:47–49. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 23. JAMA patient page. Elder abuse. Hildreth CJ, Burke AE, Golub RM. JAMA. 2011;306:568. doi: 10.1001/jama.306.5.568. [ DOI ] [ PubMed ] [ Google Scholar ]
- 24. Risk and protective factors. [Mar;2021 ]; https://www.cdc.gov/violenceprevention/elderabuse/riskprotectivefactors.html 2020
- 25. Elder mistreatment: national survey of emergency physicians. Jones JS, Veenstra TR, Seamon JP, Krohmer J. Ann Emerg Med. 1997;30:473–479. doi: 10.1016/s0196-0644(97)70007-6. [ DOI ] [ PubMed ] [ Google Scholar ]
- 26. Detecting elder abuse and neglect: assessment and intervention. Hoover RM, Polson M. https://www.aafp.org/afp/2014/0315/p453.html . Am Fam Physician. 2014;89:453–460. [ PubMed ] [ Google Scholar ]
- 27. Development and validation of a tool to improve physician identification of elder abuse: the Elder Abuse Suspicion Index (EASI) Yaffe MJ, Wolfson C, Lithwick M, Weiss D. J Elder Abuse Negl. 2008;20:276–300. doi: 10.1080/08946560801973168. [ DOI ] [ PubMed ] [ Google Scholar ]
- 28. Elder abuse: an approach to identification, assessment and intervention. Wang XM, Brisbin S, Loo T, Straus S. CMAJ. 2015;187:575–581. doi: 10.1503/cmaj.141329. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 29. Screening tools for identification of elder abuse: a systematic review. Gallione C, Dal Molin A, Cristina FVB, Ferns H, Mattioli M, Suardi B. https://doi.org/10.1111/jocn.13721 . J Clin Nurs. 2017;26:2154–2176. doi: 10.1111/jocn.13721. [ DOI ] [ PubMed ] [ Google Scholar ]
- 30. Elder neglect assessment in the emergency department. Fulmer T, Paveza G, Abraham I, Fairchild S. J Emerg Nurs. 2000;26:436–443. doi: 10.1067/men.2000.110621. [ DOI ] [ PubMed ] [ Google Scholar ]
- 31. Schofield MJ. Elder abuse. Cham, Switzerland: Springer International Publishing; 2017. Screening for elder abuse: tools and effectiveness. [ Google Scholar ]
- 32. Elder mistreatment. Swagerty DLJ, Takahashi PY, Evans JM. https://pubmed.ncbi.nlm.nih.gov/10348072/ Am Fam Physician. 1999;59:2804–2808. [ PubMed ] [ Google Scholar ]
- 33. Generational differences in knowledge, recognition, and perceptions of elder abuse reporting. Aday RH, Wallace JB, Scott SJ. Educ Gerontol. 2017;43:568–581. [ Google Scholar ]
- 34. Mandatory reporting of elder abuse: between a rock and a hard place. Rodríguez MA, Wallace SP, Woolf NH, Mangione CM. Ann Fam Med. 2006;4:403–409. doi: 10.1370/afm.575. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 35. Recognizing and reporting elder abuse and neglect. Halphen J, Varas G, Sadowsky J. https://pubmed.ncbi.nlm.nih.gov/19586086/ Geriatrics. 2009;64:13–18. [ PubMed ] [ Google Scholar ]
- 36. Emergency Medical Services Perspectives on Identifying and Reporting Victims of Elder Abuse, Neglect, and Self-Neglect. Rosen T, Lien C, Stern ME, et al. https://doi.org/10.1016/j.jemermed.2017.04.021 . J Emerg Med. 2017;53:573–582. doi: 10.1016/j.jemermed.2017.04.021. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 37. Elder abuse education in residency programs: how well are we doing? Wagenaar DB, Rosenbaum R, Page C, Herman S. Acad Med. 2009;84:611–618. doi: 10.1097/ACM.0b013e31819fb95f. [ DOI ] [ PubMed ] [ Google Scholar ]
- 38. Elder abuse. Lachs MS, Pillemer K. Lancet. 2004;364:1263–1272. doi: 10.1016/S0140-6736(04)17144-4. [ DOI ] [ PubMed ] [ Google Scholar ]
- 39. Statutes to combat elder abuse in nursing homes. Weinmeyer R. Virtual Mentor. 2014;16:359–364. doi: 10.1001/virtualmentor.2014.16.05.hlaw1-1405. [ DOI ] [ PubMed ] [ Google Scholar ]
- 40. Elder abuse in nursing homes: prevention and resolution strategies and barriers. Payne BK, Fletcher LB. J Crim Justice. 2005;33:119–125. [ Google Scholar ]
- 41. Financial abuse of the elderly in domestic setting. [Mar;2021 ];Hafemeister TL. https://www.ncbi.nlm.nih.gov/books/NBK98784/ 2003
- 42. Holding abusers accountable: an elder abuse forensic center increases criminal prosecution of financial exploitation. Navarro AE, Gassoumis ZD, Wilber KH. Gerontologist. 2013;53:303–312. doi: 10.1093/geront/gns075. [ DOI ] [ PubMed ] [ Google Scholar ]
- View on publisher site
- PDF (135.4 KB)
- Collections
Similar articles
Cited by other articles, links to ncbi databases.
- Download .nbib .nbib
- Format: AMA APA MLA NLM
Add to Collections
- Open access
- Published: 28 March 2022
Experiences of elder abuse: a qualitative study among victims in Sweden
- Mikael Ludvigsson 1 , 2 ,
- Nicolina Wiklund 1 ,
- Katarina Swahnberg 3 &
- Johanna Simmons 1
BMC Geriatrics volume 22 , Article number: 256 ( 2022 ) Cite this article
12k Accesses
20 Citations
7 Altmetric
Metrics details
Elder abuse is underreported and undertreated. Methods for prevention and intervention are being developed, but the knowledge guiding such measures is often insufficiently based on the victims’ own voices due to a paucity of studies. The aim of this study was therefore to explore experiences of elder abuse among the victims themselves.
Consecutive inpatients ≥ 65 years of age at a hospital clinic in Sweden were invited to participate, and 24 victims of elder abuse were identified. Semi-structured qualitative interviews were conducted, and transcripts were analyzed using qualitative content analysis.
The analysis generated four themes that together give a comprehensive picture of elder abuse from the participants’ subjective perspectives. The participants’ experiences of abuse were similar to previous third-party descriptions of elder abuse and to descriptions of abuse among younger adults, but certain aspects were substantially different. Vulnerability due to aging and diseases led to dependance on others and reduced autonomy. Rich descriptions were conveyed of neglect, psychological abuse, and other types of abuse in the contexts of both care services and family relations.
Conclusions
Elder abuse is often associated with an individual vulnerability mix of the aging body, illnesses, and help dependence in connection with dysfunctional surroundings. As individual differences of vulnerability, exposure to violence, and associated consequences were so clear, this implies that components of prevention and intervention should be individually tailored to match the needs and preferences of older victims.
Peer Review reports
Abuse of older adults is recognized as a pervasive and serious problem in society. Prevalence estimates have ranged from 10% upwards in cognitively intact persons from North and South America, with large variations between different countries and subcategories of the population [ 1 , 2 , 3 ]. Elder abuse is defined by the World Health Organization (WHO) as “a single or repeated act or lack of appropriate action, occurring within any relationship where there is an expectation of trust, which causes harm or distress to an older person”. It includes five different types of abuse: physical abuse, psychological abuse, sexual abuse, economic abuse, and neglect [ 4 ]. Elder abuse is associated with various adverse health outcomes including psychosocial distress, morbidity, and mortality [ 1 ]. Exposure to more than one type of abuse or by more than one perpetrator is called poly-victimization, and this common condition is generally associated with even worse health outcomes than single exposure to abuse [ 5 , 6 ]. It is also increasingly acknowledged that elder abuse is associated with previous experiences of violence in childhood and adulthood, motivating a life-course perspective in research on elder abuse [ 7 , 8 ].
The causes and mechanisms of elder abuse are important to understand, to prevent its occurrence more effectively in society. The socio-ecological model (Fig. 1 ) of abuse describes how abuse can be understood as a complex interplay between risk factors on different social levels (individual, relationship, community, or societal level) for the victim [ 5 , 9 ]. By analyzing and handling abuse with help of this model, the circumstances of abuse are concretized which facilitates practical interventions. However, experiences of elder abuse differ between professionals, other surrounding persons, and the older adults themselves [ 10 , 11 ], and the varying conceptions and definitions used have consequences for the types and forms of interventions planned. If supportive resources are not adapted to the victims’ conceptualizations of elder abuse or to their perceived needs, the resources risk being ineffective [ 1 , 12 , 13 ]. Thus, the voices of the victims themselves are important to truly understand their associated needs as well as the causes and mechanisms of elder abuse, in order to develop more effective interventions.
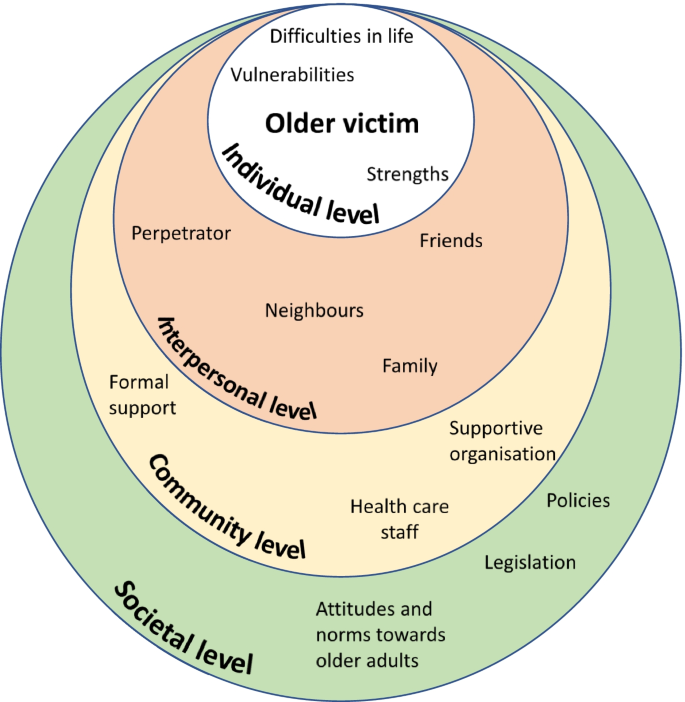
The socioecological model inspired by Bronfenbrenner [ 9 ] and Heise [ 14 ] as a mean to understand the complexity of elder abuse
Furthermore, qualitative studies have been proposed to better understand conceptual and cultural variations of elder abuse [ 1 ]. Some qualitative studies on abuse of older adults have been undertaken within a theoretical framework of intimate partner violence (IPV; [ 15 , 16 ]), but this framework differs from the framework of elder abuse for example by underestimating the categories of abused men, neglect, and abuse by personnel in healthcare or long-term care [ 17 , 18 , 19 ]. Abuse in healthcare and long-term care are particularly relevant for a comprehensive picture of elder abuse as increasing proportions of the population encounter such institutions due to increasing age, frailty, and social dependence [ 2 , 20 ].
Within the framework of elder abuse, several qualitative studies have asked professionals or other third parties about elder abuse [ 11 , 21 , 22 ], but only few have asked the victims themselves [ 21 , 23 , 24 ]. However, these few previous studies do not offer a sufficiently comprehensive picture of the matter which is why we conducted the present study.
The aim of this study was to explore experiences of elder abuse among the victims themselves. By asking the victims directly, our understanding of elder abuse can hopefully deepen and this in turn is essential for adequate prevention and intervention.
Design, setting and sample
Semi structured qualitative interviews were conducted and analyzed using content analysis. The sample was 24 participants from the larger REAGERA (Responding to Elder Abuse in GERiAtric care) project, which included developing and validating the screening instrument REAGERA-S for detecting elder abuse in healthcare [ 25 ]. Consecutive older adults ≥ 65 years of age admitted to a hospital clinic for both acute geriatric and acute medical patients were eligible for inclusion. The consecutive sampling was chosen in the pursuit of naturalistic openness, and this sampling was expected to lead to a wider range of abuse (including mild forms of abuse), compared to alternative purposeful sampling strategies. A parallel goal of gathering information-rich data was reached through a relatively large number of participants. Exclusion criteria were insufficient somatic, cognitive, or linguistic capacity to answer the screening instrument either independently or with the help of healthcare personnel. Patients at the clinic were mostly admitted from the emergency department, and the mean duration of stay for patients over 65 years was 10 days at the acute geriatric ward and 4 days at the acute medical ward during the study period. The setting is described in greater detail elsewhere [ 25 ]. Between January and June 2018, 306 potential participants were asked to participate by nurses on the ward. The screening instrument was completed by 191 participants, of which 135 were interviewed. Of these 135 participants, 24 had been victims of elder abuse and all their 24 recorded interviews were included for this qualitative study. Descriptive data about the 24 included participants are presented in Table 1 . Typically for the setting of the hospital clinic, the mean age was rather high, as were the number of medications and the degree of social dependence for managing activities of daily living—compared to an average patient in health care.
Before the interview, a nurse on the ward distributed a questionnaire to potential participants including the screening instrument REAGERA-S [ 25 ], as well as information about voluntary participation and informed consent. The screening instrument included nine questions about different kinds of abuse (e.g." Has anyone attempted to control you, limit your contact with others, or decide what you may or may not do?”;”Have you been subjected to any form of physical violence, for example being shoved, pinched, held down, hit or kicked?”), and one question about associated suffering. The instrument in total is available elsewhere [ 25 ]. No precise definition of elder abuse was presented for the participants before the interviews. Rather the information preceding the interviews included rather vague descriptions of elder abuse (e.g. “to be subjected to negative actions”) to prevent steering the participants’ thoughts or stories for the data collection. Later that same day or the following day, a qualitative interview was conducted in a private room. The interview was semi-structured using a prepared interview guide (see Supplement 1 ), with four main topics to cover (experiences of abuse, associated thoughts and feelings, effects of the abuse, and support after the abuse). The informants’ experiences of abuse are presented in this study, while their experiences of coping with abuse and their desired support are presented in a separate paper.
For the interviews, we used open-ended questions such as “Can you tell me some more about what you were exposed to?” and “What are your feelings when you think about this today?”. Probing and supplementary questions were also asked. The interviews were audio recorded and transcribed verbatim. The length of the interviews varied between 12 and 97 min. Field notes were written during or after the interviews. Just after each formal interview, the previously completed questionnaire was quickly checked for severe depression or suicidal risk. In two cases, this check – together with the interview – resulted in a referral to an appropriate care unit for support connected to being abused. The individual’s responses from the REAGERA-S were used at a later stage when classifying cases of elder abuse after the interview, described in more detail elsewhere [ 25 ]. All participants received both oral and written information about support services to contact in case of need. In addition to checking the participants’ psychological wellbeing and perceptions of participation in the interviews, additional follow-ups were carried out by phone by the researchers about 1–2 weeks after the interviews. All participants gave written informed consent at the time of participation. A potential ethical problem of the consent process was the principal vulnerability of the participant in the hospital care setting. The interviewers (three of the researchers: JS, NW and ML) usually work as physicians but were not involved in the formal care of the participants, and this was communicated to the patients orally and through a civilian clothing. By signaling thus that the interviewers were separate from the formal health care personnel, elements of vulnerability and potential dependency of the participant was prevented in the participation. Also, security and rapport were built in the meeting through active listening and validation. The study was conducted in accordance with the principles of the Declaration of Helsinki and approved by the Regional Ethics Review Board in Linköping, Sweden (2017/181–31; 2017/564–32).
Transcripts were analyzed using qualitative content analysis, based on Graneheim and Lundman [ 26 ] and a hermeneutic standpoint with an intermediate level of abstraction and interpretation [ 27 ]. For the purpose of exploring individual experiences, the qualitative content analysis was considered an appropriate method with a focus on subject, context and variation of the data [ 27 ]. The process of analysis involved the following steps: 1) repeated preliminary readings of unique interviews to obtain a sense of the whole; 2) dividing the text into units of meaning; 3) giving codes to condensed meaning units; 4) abstraction within and between interviews by aggregating codes into tentative subcategories/categories (manifest content), and subthemes/themes (latent interpretive content); 5) discussion and revision of tentative codes, subthemes/themes, and subcategories into more definitive ones. The analysis included both a search for convergent patterns and a mirror analytical strategy to investigate divergence (consideration of data that did not fit the dominant patterns) [ 28 ].
Six interviews were coded separately and were then discussed together by all the authors. For the remaining interviews, the coding and development of tentative subcategories and themes were carried out by two of the authors (ML and JS; steps 1–4). The tentative themes/subthemes were then discussed and revised (step 5) by all the authors together. This validation within the research group aimed to strengthen the research design, not by identical statements or consensus but as a form of reflexivity through contesting and supplementing each other’s readings [ 29 ]. The QSR International’s NVivo 12 software program was used as a means for sorting and managing data during the process.
The qualitative analysis generated four themes which are presented in detail below: vulnerability in old age; experiences from earlier in life; perceptions of abuse; consequences and suffering from the abuse. An overview of the themes subthemes and subcategories is depicted in Fig. 2 .
Coding tree as an overview of the themes, subcategories, and subthemes of the qualitative content analysis
Vulnerability in old age
The participants described their life situations as contexts for the adverse events they had been subjected to, and these descriptions expressed a general pattern of vulnerability. This vulnerability largely consisted of different kinds of dependence on other people: social, physical, and medical dependence. Social dependence sometimes reflected efforts to avoid loneliness, conflicts, sorrow, or other adversities for the family members.
Physical dependence could be the need to get a ride to visit friends, or a need for assistance with putting on socks due to reduced mobility, while medical dependence could be a need for assistance with injection treatment. The participants’ vulnerability was due to the natural consequences of normal aging, including a lack of energy or reduced mobility, or the consequences of illness, with reduced capacity for activities and participation. It was also a result of social relationships that had evolved over the course of a long lifetime. When participants asked for help or received help from those around them, they consequently had reduced defense against or increased vulnerability to abuse.
“Well, I’m not a happy person any longer, I’m hardly allowed to laugh, because he doesn’t like that really. […] And I also don’t get outdoors like I did before. Then I could take the bus downtown and go shopping and do whatever I wanted. Now he’s behind my wheelchair, checking me all the time, and that’s not fun.” (Woman, ID 9, 71 years).
The participants often expressed a desire to overcome their dependence, either by managing on their own or by finding alternative helpers. Thus, the dependency was often related to a specific perpetrator, but also in general related to any potential helper. However, a lack of energy or failing capacities during old age often resulted in dependence remaining. As a part of their vulnerability, the participants also expressed that it was hard to defend themselves when exposed to abusive situations:
“… if you have employees who behave a little badly to you, that’s different [that’s one thing]… But if you encounter resistance in healthcare, that’s another story.” (Man, ID 19, 85 years).
How the participants related to their vulnerability or their dependence varied, although a common approach was the desire not to bother their helpers (relatives or personnel).
“[There were] times when they [the care personnel] didn’t come. They have… they had a shortage of staff, and when some of them got sick they skipped [visiting some patients], and I was probably the one they cared about the least, as I was the most alert of us.” (Man, ID 1, 85 years).
Reduced autonomy was also described as an aspect or a consequence of dependence on help, whereby the older adults were not allowed to decide, or could not decide, about their life situation. Their autonomy was sometimes reduced by the limited willingness or ability of those around them to meet their needs. On other occasions, their autonomy was reduced by their physical or social impairments. For example, they were sometimes not allowed to decide where to live, or which activities to engage in.
“And they’re talking about putting me there again [in the nursing home], and I don’t want that, but what the hell can I do [about it]?” (Man, ID 1, 85 years).
The participants also expressed their perceptions of limited autonomy when they were treated like objects rather than individuals, or when the personnel did not show any interest or engagement in their personal needs, desires, or personality. For instance, all residents at the nursing home were invited – or sometimes rather forced – to participate in certain specific activities, due to the mistaken ageist notion that all older adults enjoy the same sort of activities. Thus, the older adults perceived reduced autonomy when grudgingly participating in bingo competitions.
The participants also conveyed their theories about why their dependence became so problematic, and these theories were often about specific members of staff being perceived as unfriendly or incompetent. Other theories related to how structural deficiencies of society – or of healthcare, or of certain organizations – contributed to a general lack of humanity among the older adults’ potential helpers. An example of such a perceived structural deficiency is when financial savings made by an organization are allowed to trump care quality or staff competence in healthcare. Accordingly, a recurrently suggested intervention to prevent elder abuse would be to educate the care staff:
Interviewer: “How would it be possible to … [prevent age-discriminatory care by the assisted living]? Participant: “By educating the care staff, of course…. So to [that they would] understand that an older adult has a background whatever that may be./…/. Perhaps education [for them], to understand the individual, so to say”. (Woman, ID 3, 84 years).
Experiences from earlier in life
In addition to the above descriptions of vulnerability during old age, the participants also spoke about their earlier lives, including time of adversity and joy. Several older participants described that, during old age and beforehand, they could receive strength or support from a friend or a partner, from family members, or by participating in an organization. These surrounding supporting elements helped to create security and meaningfulness, despite the adversities of life.
“She [my wife] was valuable to me… in all kinds of ways. And I have always encountered love through church, and these things have been very valuable to me.” (Man, ID 19, 85 years).
Some participants highlighted their activities or professional experiences that had provided support in life, while others highlighted important insights or mental attitudes that had helped to form their identities, their inner strengths, or their sense of meaning in life.
“When I grew up […] I had to do as I was told. And with this attitude I have managed.” (Man, ID 6, 76 years)
Alongside the participants’ stories about positive experiences and support throughout life, they also conveyed rich stories about difficulties and adversities in life. These stories were often about being a victim of violence during childhood, for example being subjected to school bullying or experiencing different types of violence in the family.
“I was five years old when I saw my father threaten her [my mother] with a loaded rifle, then she was wedged into a corner and he stood in the middle of the floor. […] Then my childhood ended, that day.” (Woman, ID 8, 73 years).
The participants told their stories about being subjected to violence in the past with such passion and emphasis that it became clear during the interviews how violence – even many years ago – could have just as strong an impact on health as recent events of victimization.
Perceptions of abuse
In the interviews, the participants described all five types of abuse. Patterns of neglect and psychological violence were most prominent in their stories, while economic, physical, and sexual violence were generally less prominent.
Neglect occurred in relation to different helpers that the participants were dependent on, and the neglect was related to a variety of needs. Hygiene needs were neglected when the participants had limited access to help with showering, cleaning or washing services, or clothing. Insufficient assistance with buying food or medication was described in association with staff shortages at the care organizations, which could prevent the older adults from initiating treatment prescribed by a doctor.
Neglected medical needs could involve sloppy or incompetent wound dressing, or when staff often forgot to administer medications. Several stories related to how care staff dismissed the older adults’ medical needs or symptoms, on the incorrect ageist assumption that the symptoms were signs of normal aging. The following quotation was interpreted as an example of age discrimination, and at the same time neglect of medical needs when a woman was refused a regular treatment regime. It was unclear whether the neglect was intentional or not.
“I was in France last year. I went down a mountain, skiing, it was slippery. [I] was going down and then got stuck in a fence, and so I twisted my knee. […] [I waited two days to seek healthcare until I came home from the journey.] And then they tell me ‘Well, because of your age you’ll have to wait for six months [to receive care]’, oh my god, and ‘You’ll have to do physiotherapy and attend to the osteoarthritis school’.” (Woman, ID 18, 69 years).
Examples of social needs being neglected varied in nature. This could involve older adults being frequently forgotten, after staff had said “I’ll be right back” in response to a request for help. Alternatively, social needs could be neglected when older residents at a nursing home were forced to attend social activities that were not in line with the individual’s specific preferences or abilities. A lack of staff continuity could mean that the participants were deprived of steady relationships with other people. In such ways, the participants expressed a lack of a meaningful existence, secondary to the social neglect.
“And the nursing home was so… well, it was so boring, damn it! It was as if a lot of… I don’t know what to call it… zombies [demented people] went around. They didn’t talk. That [living situation] wasn’t stimulating, either for me or for them.” (Man, ID 1, 85 years).
Psychological abuse was often connected to neglect and occurred in healthcare as well as in nursing homes and in family environments. The psychological abuse was often perceived as a means by which to control or manipulate the participant’s actions. This control could be about small matters, like the choice of which food to eat, but it could also be about more important matters like whether or not to request home service. Sometimes the abuser used aggressive speech if the participant did not live up to the abuser’s expectations or demands.
“I’ve talked to him about it [getting home service], but he doesn’t want that, because he thinks it’s too expensive. But I just feel I don’t have energy to do anything. And he says [to me]: ‘You’re so damned lazy.’” (Woman, ID 9, 71 years).
Control was sometimes exerted verbally, but often involved more subtle non-verbal expressions, such as constant surveillance in daily activities, or expressing a non-verbal tone of disapproval if the participant met friends. In one case, a woman had even been prevented from seeing her mother on her death bed:
“So when my mother was dying, they called me [from her town] and told me to come as there was not much time left. […] I’ll come right away I said, I’ll get on the first flight. And then my husband told me I couldn’t go as it was the weekend, and that I should wait until Monday. […] I wanted to say goodbye [to her] anyway, I wanted to be with her. But I never got there in time, they called me on Monday morning and said she was gone. […] And I hate this.” (Woman, ID 7, 66 years).
The controlling behavior often turned into direct threats against the participant from a child or a partner. These threats could be related to physical violence or not being allowed to see their grandchildren anymore. Psychological abuse also occurred in care environments, although the expressions were generally less explicit. In healthcare, just as in family environments, the abuse was perceived as an attempt to control the older participant’s behavior. Often the intent of the staff seemed to be well-meaning, but the expression was perceived aggressive or otherwise negative by the participant. One example was the following situation, where the participant had just completed a cardiac exercise test at the hospital:
“… I had cycled very fast, I was in severe pain and I was lying on the bed. […] and then she [the member of staff] would, at the physician’s request, spray nitro medication under my tongue, which she did and said to me: ‘Shut your mouth and swallow’, but I couldn’t because I was just in cramp… so she says again ‘Shut your mouth and swallow!’ but I still couldn’t do it, and then she turns away and says ‘Well then, forget that shit!’.” (Woman, ID 8, 73 years).
The descriptions of economic abuse that emerged during the interviews were many and rich in character. Sometimes the perception of economic abuse was not primarily associated with the lost financial value, but rather with the feeling of deception after a theft within a relationship of trust, or the feeling of sorrow when the lost item had great sentimental value.
“I felt terrible [when the jewelry was stolen by service staff], and after that I have never again… asked [them] for help. […] Yes, I think a lot about the jewelry being gone… it was a necklace that I had inherited from my mother, and a bracelet…” (Woman, ID 23, 73 years).
Stories about physical abuse during aging were few, but there were more examples of this from earlier in life. Examples of physical violence in old age including a robbery necessitating hospital care, being pushed by an official during a home visit, physical violence from a fellow passenger during transportation services, and one participant being hit by hospital staff.
“I’ve been hit on the head with a pillow. Just because I was cranky, she [the nurse] said. And I didn’t like that… And I said: ‘Now you get out of here, because you shouldn’t be working with people.’ […] [I] think it is frightening when you have to go to a care facility to receive care, and then you get hit! I don’t think it is acceptable.” (Man, ID 6, 76 years).
There were several stories about sexual abuse from earlier in life, but only few from old age. In one case the participant had been recurrently raped within the marriage, but the raping had ended some years before the age of 65. In another case, sexual abuse in contact with healthcare staff had obviously occurred during old age.
“Once, there was a physician that made some – it sounds weird now that I’m 84, I think I was ten years younger then – he really made sexual invitations [to me]. Yes, I think it sounds weird, but I felt very awkward.” (Woman, ID 3, 84 years).
The participants’ stories of sexual abuse expressed clearly feelings of shame and disgust.
Consequences and suffering from the abuse
The abuse that the participants had been exposed to led to various consequences. Psychological consequences included uncomfortable or painful feelings or thoughts that tormented the participant long after the abuse. For example, this could include nervousness, depression, disappointment, or guilt on the part of the abuser or the victim. The intensity of these uncomfortable feelings and thoughts varied over time, with a common gradual decrease as time, ordinary life, or support measures had helped to sooth the remaining discomfort. However, even a long time after the abuse had ended, the painful feelings and thoughts could be brought back by events or conversations, so that the intensity became strong again. Even if the interviews themselves evoked such painful feelings, the participants generally perceived the interviews as positive.
“… Because I sense this, how can somebody just do that? It’s [the painful experience]… Yes, it’s inside me. I try to get rid of it when it comes, but it isn’t so easy, sometimes it just comes and yes, it’s just there.” (Woman, ID 10, 67 years).
The participants described feelings of inferiority or uselessness, even though they tried to convince themselves that such feelings or thoughts were not truthful. Feelings of nervousness and fear increased again when experiencing new threats of abuse, for example when facing a new need for hospital care after previous negative experiences of abuse in healthcare.
“I hate being admitted [to hospital] like this, you don’t know which department you will be admitted to or which staff you will meet. […] You’re always prepared for the worst. You never know who you will meet when you’re admitted… Of course, I’m always on my guard… against a punch or such things.” (Man, ID 6, 76 years).
The fear of being robbed again made the participants vigilant and distrustful toward staff, strangers, and authorities. Lasting harm from abuse could include aches due to internal tension. Although the participant conveyed that the physical symptoms were caused by the abuse or medical errors, such causal relationships or physical consequences sometimes seemed uncertain for the researchers.
Social effects of the abuse could include loneliness, avoiding going outdoors due to fear of violence, or social isolation caused by reduced self-confidence or an abuser limiting their personal freedom. Social effects could also include a reluctance to accept care service due to fear, even though the older adult needed such services. Regardless of whether the abuse was ongoing or in the past, the suffering could be so intense that the person had lost the will to live or even planned to take their own life.
“I wouldn’t be alive if I didn’t have them [the children]. Then [without the children] I’d have been gone [dead] a long time ago. Then, I wouldn’t be alive. I don’t like life that much.” (Woman, ID 7, 66 years).
The participants commonly expressed feelings of abandonment and lack of control, in association with the abuse and their situation. By contrast, a few participants instead conveyed how they continued to defend their autonomy and strove to keep control of the situation through different strategies, despite their limited physical condition due to old age.
Discussion and implications
This aim of this study was to explore experiences of elder abuse among the victims themselves, as their own descriptions can help us to better understand how to develop prevention and interventions against elder abuse. The qualitative analysis resulted in four different themes (vulnerability in old age; experiences from earlier in life; perceptions of abuse; and consequences and suffering from the abuse), which describe different aspects of abuse from the participants’ subjective perspectives. In all, many of the participants’ perceptions of abuse were similar to previous descriptions by third party of elder abuse [ 11 , 21 , 22 ]. Some aspects of the descriptions of elder abuse in this study were also similar to previous descriptions of abuse among younger adults, but other aspects were substantially different [ 30 , 31 , 32 ], as discussed below.
Vulnerability in old age and experiences from earlier in life
Vulnerability to abuse during old age was described as different sorts of dependence on other people, and a lack of autonomy. Due to the effects of normal aging or accumulated diseases, the participants had limited mobility and an increasing need for care in everyday life, which meant dependence on care and vulnerability to abuse from others.
When the participants were exposed to abuse, their ability to defend themselves was also low for the same reasons. In general, this contributed to a submissive attitude toward the helper, together with inner reactions of anger, sorrow, and resignation. These descriptions of vulnerability have similarities with descriptions of vulnerability and powerlessness among younger adult victims of abuse in healthcare and other settings [ 32 , 33 ]. At the same time, the context of the aging body is characteristically different for the older adult, with decreasing capabilities and increasing dependence on care. The participants’ vulnerabilities were very varying and unique to each individual in terms of aging, morbidity, and life experiences.
The descriptions of vulnerability in old age were similar to those recounted by Y Mysyuk, RG Westendorp and J Lindenberg [ 23 ]. Dependence was described as a reciprocal process between the abuser and the victim in Mysyuk et al., something that was not spontaneously conveyed from the participants of this study. Nor did we identify the pattern described in Mysyuk et al., whereby increased weakness or dependence would provoke more violence.
The participants’ stories about previous stages of their life contributed to comprehensive individual pictures of how specific abuse in old age had had impact on their health. It was particularly evident that abuse in the past could have a great impact on health in old age, for example when psychological abuse in childhood had additive or synergistic effects on the perception of elder abuse. This is in line with previous literature on poly-victimization, and underlines that understanding elder abuse presupposes considering previous victimization as well as personality and the victims’ experiences of support, attachment styles, and challenges in life [ 5 , 8 , 34 ]. According to the socio-ecological model of abuse (Fig. 1 ), vulnerability can occur on all levels of an individual’s life, although previous experiences of life mainly correspond to the individual and interpersonal levels for the older adult [ 5 , 9 ]. Previous life experiences are important not only for understanding the individual’s unique vulnerability to abuse, but also for considering the victim’s individual strengths and resources when designing interventions and the prevention of elder abuse [ 35 ]. Hence, our results agree well with previous findings that a life-course perspective is essential when trying to understand the causes and consequences of elder abuse [ 6 , 7 , 8 ]. However, our findings also underline that abuse occurs in a context, and factors on all levels of the socioecological model influence the experience of abuse, e.g., ageist attitudes and dysfunctional care organizations described further on. By paying attention to and validating the older adult’s own life story, staff can indirectly contribute to interventions at community level in accordance with the socio-ecological model, as this level includes how the victim is treated by organizations [ 19 ].
Different kinds of elder abuse, ageism, and perceived causes of elder abuse
Neglect was a common kind of abuse in this study, and there were rich descriptions of this from healthcare settings and long-term care institutions. Not only were physical and medical needs neglected – so, too, were social needs, with consequent intense feelings of abandonment and lack of control among the participants. These descriptions were partly similar to those found in previous studies [ 36 ], although the examples of neglect in this study were often modest in character, meaning potentially mild physical adverse effects in the short term. Nevertheless, also modest shortcomings with hygiene or cleaning could have serious or even life-threatening consequences, as they meant an increased risk of serious wound infections. Ageist attitudes were obvious in different types of abuse, and especially in the descriptions of neglect, in which for example all older adults were treated like objects in a routine way without respect for their individual characters, needs, or preferences.
The psychological abuse occurred in both family and care environments and seemed to correspond to the abusers’ attempts to control the participants’ behaviors. In care environments, the abuse could be a way for staff to control behaviors in line with specific care routines or comfortable forms of work for the staff. The descriptions of psychological abuse in this study were similar to previous descriptions of psychological abuse in younger victims in healthcare and in younger persons in other environments [ 30 , 33 , 37 ].
The participants often added their own personal explanations for the abuse. In addition to descriptions of vulnerability and self-blame, common explanations included individual staff members being unfriendly, care organizations being structurally dysfunctional (with a lack of competence and resources), general greed at all levels of society, and discriminatory (ageist) attitudes and actions leading to neglect. Similar explanations have been described in previous studies, with ageism probably corresponding to all levels of the socio-ecological model [ 11 , 23 , 38 , 39 ]. Some people would perhaps think that structural deficiencies are not relevant to abuse, but the very definition of elder abuse by WHO clarifies that also “lack of appropriate action” in a dysfunctional environment can constitute elder abuse [ 4 ].
A general issue from the analysis of the interviews was whether the WHO definition of elder abuse is too narrow since it limits elder abuse to relations of trust. In several examples there was no identified relation of trust in a reported situation, but rather a “situation of trust” in which the abusive action would best be described as an example of elder abuse. For example, when an older adult is exposed to abuse during transportation services, there would be a situation of trust regardless of whether there are any relations of trust. The older adult would typically be vulnerable in this situation due to the physical limitations of ageing. With a narrow interpretation of the WHO definition, this abuse would dysfunctionally not be classified as elder abuse, although the theoretical framework of elder abuse would fit for an adequate understanding and prevention of the same abuse [ 40 ].
Consequences of the abuse
The participants described consequences of abuse in a way that resembled how consequences of trauma have been previously described among both older and younger adults [ 3 , 30 , 41 ]. Whereas patterns of psychological consequences (with negative thoughts and feelings of shame and fear) were rather like descriptions from previous studies among younger adults, the behavioral consequences were different and related to various social and physical preconditions among the older adults compared to younger adults. Social isolation and loneliness were natural consequences of limited mobility in normal aging or disease, and when abuse also contributed to these limitations the sense of isolation grew particularly strong. When participants chose not to receive home-care services because of the fear of recurrent abuse – despite their needs for assistance – the limiting consequences of abuse were particularly evident. There were also examples from the interviews of how neglect could have serious potential physical consequences, as many of the older adults were less physically able to withstand medical mistreatment.
Implications for the prevention of and intervention into elder abuse
Our findings have several implications for the prevention of and intervention into elder abuse. In terms of the socio-ecological model, preventive measures at community (including hospital level) and societal levels could be to ensure a minimum standard (for example by using legislation or economic incentives) for the care of older adults. According to the participants' voices, higher minimum standards of staff competence and resources would be likely to reduce the tendencies toward neglect, psychological abuse, or other kinds of abuse. Vulnerability and abuse could according to the participants also be prevented through education to care staff about different aspects of elder abuse and about aging. Such educational measures were suggested to promote person-centredness and prevent ageist attitudes, as these attitudes seem to contribute to both the vulnerability and elder abuse [ 39 ]. In addition, support units are also needed to offer individual assistance to victims of elder abuse as the negative consequences are substantial. According to a bifocal ecological approach, the assistance should not only be directed to the victim for an effective prevention but also to the perpetrator [ 42 ]. However, an important principle should be to adapt the preventive measures to the individual, as both vulnerability and abuse perceptions vary significantly according to the individual’s unique biopsychosocial conditions and experiences from earlier life. This also underlines the need for a life-course perspective on elder abuse [ 34 , 43 ].
Limitations
In order to minimize bias introduced by the researchers’ preconceptions and instead promote reflexivity, four researchers with different backgrounds have cooperated in the study. Three of the authors work as physicians within geriatrics and psychiatry, while the fourth author works with research, mostly outside hospital environments.
The fact that the sample was selected from inpatient care could be regarded as a disadvantage, as some older adults might have had too little energy to participate actively in interviews while suffering from an acute illness with associated physical exhaustion. On the other hand, the decision to recruit participants from inpatient care meant certain advantages, for example offering the participants a secure context for the interviews while their home or other environments might have been less secure, or more easily controlled by an abuser.
The results are likely to be transferable to older adults in Sweden but should be transferred with caution to countries with other cultures or societal structures.
This is one of few studies to date in which qualitative interviews have been used to explore experiences of elder abuse among the victims themselves. Their stories had similarities with both previous third-party descriptions of elder abuse and previous descriptions of abuse among younger adults. There were also substantial differences, with the consequence that elder abuse needs to be understood and managed by partly different means compared to abuse among younger adults. Vulnerability to elder abuse is often associated with an individual mix of the aging body, illnesses, and a dependence on secondary help. A life-course perspective considering experiences from the individual’s past would be beneficial when designing support for older victims, as such experiences are important to the degree of suffering and disability that the victim develops in relation to elder abuse. Prevention ought to include individually tailored help or support to reduce vulnerability, specific education, and ensuring an acceptable minimum standard of care for older adults in general [ 14 ].
Availability of data and materials
The datasets generated and analyzed during the current study are not publicly available and are not available from the corresponding author on request due to reasons concerning participant privacy and confidentiality.
Dong XQ. Elder Abuse: Systematic Review and Implications for Practice. J Am Geriatr Soc. 2015;63(6):1214–38.
Article Google Scholar
Yon Y, Ramiro-Gonzalez M, Mikton CR, Huber M, Sethi D. The prevalence of elder abuse in institutional settings: a systematic review and meta-analysis. Eur J Public Health. 2019;29(1):58–67.
Lachs MS, Pillemer KA. Elder Abuse. N Engl J Med. 2015;373(20):1947–56.
Article CAS Google Scholar
World Health Organisation. Elder Abuse: Fact sheet. Retrieved February 6th, 2021 from https://www.who.int/news-room/fact-sheets/detail/elder-abuse (2020).
Teaster PB. A framework for polyvictimization in later life. J Elder Abuse Negl. 2017;29(5):289–98.
Simmons J, Swahnberg K. Lifetime prevalence of polyvictimization among older adults in Sweden, associations with ill-heath, and the mediating effect of sense of coherence. BMC Geriatr. 2021;21(1):129.
Easton SD, Kong J. Childhood Adversities, Midlife Health, and Elder Abuse Victimization: A Longitudinal Analysis Based on Cumulative Disadvantage Theory. J Gerontol B Psychol Sci Soc Sci. 2021;76(10):2086–97.
Kong J, Easton SD. Re-experiencing Violence Across the Life Course: Histories of Childhood Maltreatment and Elder Abuse Victimization. J Gerontol B Psychol Sci Soc Sci. 2019;74(5):853–7.
Bronfenbrenner U. The ecology of human development : experiments by nature and design. Cambridge, Mass.: Harvard Univ. Press; 1979.
Hempton C, Dow B, Cortes-Simonet EN, Ellis K, Koch S, LoGiudice D, Mastwyk M, Livingston G, Cooper C, Ames D. Contrasting perceptions of health professionals and older people in Australia: what constitutes elder abuse? Int J Geriatr Psychiatry. 2011;26(5):466–72.
Killick C, Taylor BJ, Begley E, Carter Anand J, O’Brien M. Older people’s conceptualization of abuse: a systematic review. J Elder Abuse Negl. 2015;27(2):100–20.
Harbison J, Coughlan S, Beaulieu M, Karabanow J, Vanderplaat M, Wildeman S, Wexler E. Understanding “elder abuse and neglect”: a critique of assumptions underpinning responses to the mistreatment and neglect of older people. J Elder Abuse Negl. 2012;24(2):88–103.
Feltner C, Wallace I, Berkman N, Kistler CE, Middleton JC, Barclay C, Higginbotham L, Green JT, Jonas DE. Screening for Intimate Partner Violence, Elder Abuse, and Abuse of Vulnerable Adults: Evidence Report and Systematic Review for the US Preventive Services Task Force. JAMA. 2018;320(16):1688–701.
Heise LL. Violence against women: an integrated, ecological framework. Violence Against Women. 1998;4(3):262–90.
Montminy L. Older women’s experiences of psychological violence in their marital relationships. J Gerontol Soc Work. 2005;46(2):3–22.
Eisikovits Z, Band-Winterstein T. Dimensions of Suffering among Old and Young Battered Women. Journal of Family Violence. 2015;30(1):49–62.
Hightower J, Smith MJ, Hightower HC. Hearing the voices of abused older women. J Gerontol Soc Work. 2006;46(3–4):205–27.
Pathak N, Dhairyawan R, Tariq S. The experience of intimate partner violence among older women: A narrative review. Maturitas. 2019;121:63–75.
Weeks LE, Leblanc K. An ecological synthesis of research on older women’s experiences of intimate partner violence. J Women Aging. 2011;23(4):283–304.
Bruggemann AJ, Wijma B, Swahnberg K. Abuse in health care: a concept analysis. Scand J Caring Sci. 2012;26(1):123–32.
Meyer SR, Lasater ME, Garcia-Moreno C. Violence against older women: A systematic review of qualitative literature. PLoS One. 2020;15(9):e0239560.
Erlingsson CL, Carlson SL, Saveman BI. Perceptions of elder abuse: voices of professionals and volunteers in Sweden--an exploratory study. Scand J Caring Sci. 2006;20(2):151–9.
Mysyuk Y, Westendorp RG, Lindenberg J. How older persons explain why they became victims of abuse. Age Ageing. 2016;45(5):696–702.
Yan E. Elder Abuse and Help-Seeking Behavior in Elderly Chinese. J Interpers Violence. 2015;30(15):2683–708.
Simmons J, Wiklund N, Ludvigsson M, Nagga K, Swahnberg K. Validation of REAGERA-S: a new self-administered instrument to identify elder abuse and lifetime experiences of abuse in hospitalized older adults. J Elder Abuse Negl. 2020;32(2):173–95.
Graneheim UH, Lundman B. Qualitative content analysis in nursing research: concepts, procedures and measures to achieve trustworthiness. Nurse Educ Today. 2004;24(2):105–12.
Graneheim UH, Lindgren BM, Lundman B. Methodological challenges in qualitative content analysis: A discussion paper. Nurse Educ Today. 2017;56:29–34.
Patton MQ. Qualitative research and evaluation methods. Thousand Oaks, Calif.: Sage Publications; 2002.
Malterud K. Qualitative research: standards, challenges, and guidelines. Lancet. 2001;358(9280):483–8.
Sleutel MR. Women’s experiences of abuse: a review of qualitative research. Issues Ment Health Nurs. 1998;19(6):525–39.
Lim BH, Valdez CE, Lilly MM. Making Meaning Out of Interpersonal Victimization: The Narratives of IPV Survivors. Violence Against Women. 2015;21(9):1065–86.
Thomas KA, Joshi M, Wittenberg E, McCloskey LA. Intersections of harm and health: a qualitative study of intimate partner violence in women’s lives. Violence Against Women. 2008;14(11):1252–73.
Swahnberg K, Wijma B, Hearn J, Thapar-Bjorkert S, Bertero C. Mentally Pinioned: men’s perceptions of being abused in health care. Int JMen’s Health. 2009;8:60.
Storey J, Perka M. Reaching Out for Help: Recommendations for Practice Based on an In-Depth Analysis of an Elder Abuse Intervention Programme. Br J Soc Work. 2019;49(5):1370–1370.
Ramsey-Klawsnik H, Miller E. Polyvictimization in later life: Trauma-informed best practices. J Elder Abuse Negl. 2017;29(5):339–50.
del Carmen T, LoFaso VM. Elder neglect. Clin Geriatr Med. 2014;30(4):769–77.
Swahnberg K, Thapar-Bjorkert S, Bertero C. Nullified: women’s perceptions of being abused in health care. J Psychosom Obstet Gynaecol. 2007;28(3):161–7.
Walsh CA, Olson JL, Ploeg J, Lohfeld L, MacMillan HL. Elder abuse and oppression: voices of marginalized elders. J Elder Abuse Negl. 2011;23(1):17–42.
Pillemer K, Burnes D, MacNeil A. Investigating the connection between ageism and elder mistreatment. Nature Aging. 2021;1(2):159–64.
Goergen T, Beaulieu M. Critical concepts in elder abuse research. Int Psychogeriatr. 2013;25(8):1217–28.
Pless Kaiser A, Cook JM, Glick DM, Moye J. Posttraumatic Stress Disorder in Older Adults: A Conceptual Review. Clin Gerontol. 2019;42(4):359–76.
Joosten M, Vrantsidis F, Dow B. Understanding Elder Abuse: A scoping study. Melbourne: University of Melbourne and National Ageing Research Institute; 2017.
Google Scholar
Mosqueda L, Burnight K, Gironda MW, Moore AA, Robinson J, Olsen B. The Abuse Intervention Model: A Pragmatic Approach to Intervention for Elder Mistreatment. J Am Geriatr Soc. 2016;64(9):1879–83.
Download references
Acknowledgements
Not applicable.
Open access funding provided by Linköping University. This work was supported by the Swedish Crime Victim Fund, grants no. 3322/2017, 2944/2018, and 03384/2019. The funding source had no involvement in the study design, data collection, analysis, interpretation of the data nor in writing the manuscript.
Author information
Authors and affiliations.
Department of Acute Internal Medicine and Geriatrics and Department of Health, Medicine and Caring Sciences, Linköping University, Linköping, Sweden
Mikael Ludvigsson, Nicolina Wiklund & Johanna Simmons
Department of Psychiatry and Department of Biomedical and Clinical Sciences, Linköping University, Linköping, Sweden
Mikael Ludvigsson
Department of Health and Caring Sciences, Faculty of Health and Life Sciences, Linnaeus University, Kalmar, Sweden
Katarina Swahnberg
You can also search for this author in PubMed Google Scholar
Contributions
All authors contributed to the design of the study. JS, NW and ML performed the interviews and performed proofreading of transcripts. Six interviews were coded separately and were then discussed together by all the authors. For the remaining interviews, the coding and development of tentative subcategories and themes were carried out by ML and JS. Tentative themes/subthemes were then discussed and revised by all the authors together. ML wrote the first draft of the manuscript, and all authors contributed to and approved the final manuscript.
Corresponding author
Correspondence to Mikael Ludvigsson .
Ethics declarations
Ethics approval and consent to participate.
The study was approved by the Regional Ethics Review Board in Linköping, Sweden (2017/181–31; 2017/564–32) and was conducted in accordance with the principles of the Declaration of Helsinki. All participants gave written informed consent at the time of participation.
Consent for publication
Not applicable .
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file1..
Supplement 1. INTERVIEW GUIDE (for two parallel studies).
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Ludvigsson, M., Wiklund, N., Swahnberg, K. et al. Experiences of elder abuse: a qualitative study among victims in Sweden. BMC Geriatr 22 , 256 (2022). https://doi.org/10.1186/s12877-022-02933-8
Download citation
Received : 12 October 2021
Accepted : 10 March 2022
Published : 28 March 2022
DOI : https://doi.org/10.1186/s12877-022-02933-8
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Mistreatment
BMC Geriatrics
ISSN: 1471-2318
- General enquiries: [email protected]

IMAGES
COMMENTS
This collection contains all stories of abuse that have been featured in the Victim, Family & Caregiver Resources: Neglect & Abandonment, Sexual Abuse, Physical Abuse, Psychological Abuse, and Financial Exploitation.
Examples of Case Studies on Elder & Nursing Home Abuse 1. Suspected Nursing Home Abuse in Massachusetts. After hundreds of 911 calls were made about suspected nursing home abuse, a criminal investigation was launched against an assisted living facility in Watertown. Several of the heartbreaking reports include:
This case report examines the suspected elder mistreatment in an aphasic, septic patient under the care of family members, one of which was also his medical decision maker.
CASE STUDY 1. For several weeks, church members noticed that Mr. L, 82 years of age, had bruises, cuts, and scrapes on his face, hands, and arms. Mr. L always had some plausible explanation and, knowing that he was the sole caretaker for his very ill wife of 61 years, they did not press the issue.
1) A 75‐year old man with pulmonary fibrosis is admitted for pneumonia. As you are going towards his room to give him his medications, you hear his partner say to him in a nasty tone of voice: “Stop being so stubborn. I need you to give me access to your bank accounts.
This video explores the issues of family abuse against an older adult very personally from the point of view of five different victims. Their candor in telling about their situation gives the viewer insight into the ambivalent feeling of older abuse victims as they try to find resolution to their pain.
Outlined below are a selection of case studies provided by centres across Australia that demonstrate the issues faced by people experiencing elder abuse and the vital work undertaken by centres to support their clients and communities.
Understanding Senior Abuse: Facts, Tips, Contacts. Ask the group for their perspective: • Is it abuse? • Is it clearly one kind of abuse or possibly a combination? • Would anyone hesitate to name the abuse? If so, why? Encourage the participants to name their reasons. Ask them to look at those reasons from another point of view.
Elder abuse can present in many forms, including physical abuse, psychological/emotional abuse, sexual abuse, financial abuse, and neglect. Many studies estimate that about 10% of all people over the age of 65 experience some form of abuse.
Consecutive inpatients ≥ 65 years of age at a hospital clinic in Sweden were invited to participate, and 24 victims of elder abuse were identified. Semi-structured qualitative interviews were conducted, and transcripts were analyzed using qualitative content analysis.